-
PDF
- Split View
-
Views
-
Cite
Cite
Alessandro Boscarelli, Edoardo Guida, Giulia Ceschiutti, Benedetta Bossini, Damiana Olenik, Egidio Barbi, Jürgen Schleef, Lipoblastoma as a cause of secondary omental torsion in children: report of the first case, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab151, https://doi.org/10.1093/jscr/rjab151
Close - Share Icon Share
Abstract
Acute abdominal pain remains a major diagnostic challenge to date. Omental torsion is an infrequent cause of abdominal pain in children, which usually presents with non-specific symptoms. Herein, we report a case of persistent abdominal pain after a minor abdominal trauma. A solid mass was found in the lower abdomen at ultrasound imaging evaluation. Surgical exploration demonstrated an omental torsion secondary to a rare neoplasm of childhood.
INTRODUCTION
Omental torsion is an uncommon cause of abdominal pain, which can often mimic other acute surgical pathologies such as appendicitis, cholecystitis or Meckel diverticulum [1]. Omental torsion is defined as twisting of the omentum on its long axis, which can lead to reduced blood supply to its distal part and to acute hemorrhagic infarction of the tissue. It can be primary or secondary depending on the presence or not of an underlying anomaly (ordinarily, a cystic lesion) at the distal end of the omentum [2].
Herein, we describe a singular case of secondary omental torsion accidentally discovered at surgical exploration in a child with persistent pain following a blunt abdominal trauma.
CASE REPORT
A 4-year-old girl presented to our Paediatric Emergency Department for persistent lower quadrants abdominal pain following a blunt abdominal trauma, which occurred few hours before while playing with other children in a public park. Remarkably, the abdominal pain was described as a constant pressure associated with urge to urinate. The patient’s past medical history was uneventful. Physical examination was unremarkable except for a tenderness of lower abdomen. Blood tests showed a neutrophilic leucocytosis (white blood cell (cells/mm3): 14 810; neutrophils (%): 71) and elevated levels of C-reactive protein (122 mg/L). An abdominal ultrasound (US) scan was performed, demonstrating a hyperechoic and inhomogeneous solid mass (10 x 4 x 8 cm), located cranially to the bladder with no vascular signal at color doppler. Remarkably, the left ovary was not visualized at the US scans. Tumor markers on blood test revealed high level of cancer antigen125 (220.9 IU/ml), while levels of beta human chorionic gonadotropin, alphafeto-protein and carcinoembryonic antigen were within normal limits. Due to the laboratory findings, broad-spectrum antibiotic therapy was started. Suspecting an ovarian mass and/or adnexal torsion, the patient underwent abdominal exploration through a Pfannenstiel incision. Both ovaries appeared in normal status, and a solid well-encapsulated mass originating from the great omentum twisted around his vascular peduncle was found (Fig. 1). Histologic examination of the mass revealed a large encapsulated lipoblastoma arising from the greater omentum which was totally excised (Figs 2 and 3), and cytogenetic analysis did not show any chromosomal rearrangements. The postoperative course was unremarkable. The patient was discharged home on postoperative day 5. Sonographic follow-up and levels of cancer antigen125 repeated at 3 months postoperatively were normal.
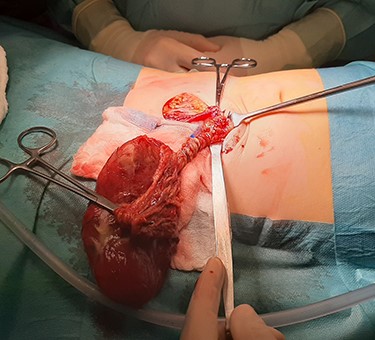
Intraoperative view of an omental torsion owing to a lipoblastoma of the greater omentum.
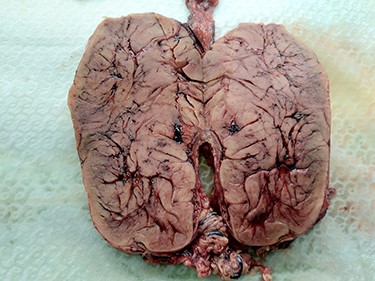
Close-up view of the macroscopic appearance of internal structure of the omental lipoblastoma.
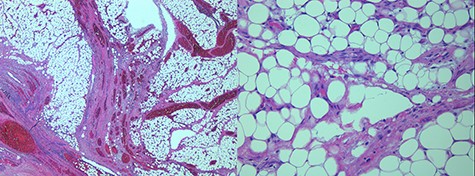
Microscopic images of the omental lipoblastoma taken through a 2.5X (left) and 20X (right) objectives on hematoxylin and eosin-stained histological sections.
DISCUSSION
Acute abdominal pain is a diagnostic challenge, especially in the pediatric age. Omental torsion is rarely described as a cause of acute abdominal pain, and the first case of torsion of the greater omentum was reported by De Marchette in 1851 [3].
Omental torsion is a condition characterized by twisting of the greater omentum around a pivotal point usually in a clockwise direction, thus compromising its vascularity. Interestingly, the majority of omental torsions are observed in the right side of the abdomen with the omentum twisted around the distal right epiploic artery [2, 3]. Omental torsion is extremely rare in pediatric age (0.1% of the cases who underwent surgery for acute appendicitis), with more than 85% of cases reported in adults and a peak incidence between the fourth and fifth decade of life [4].
Omental torsion can be primary or secondary. In particular, primary omental torsion occurs without evidence of an underlying pathology. Predisposing factors for primary omental torsion include anatomical anomalies, traumatic events, hyperperistalsis, variations of intra-abdominal pressure or augmented fat deposition. On the other hand, secondary omental torsion is associated with preexisting pathology such as masses (e.g. simple or hydatid cysts, lymphangiomas), hernias and adhesions [5]. Accompanying symptoms of an omental torsion are usually nonspecific, and they include abdominal pain, nausea, vomiting, and/or low-grade fever. A mild leukocytosis and a palpable abdominal mass may be also encountered [6]. In our case, the child was referred to our Paediatric Emergency Department for persistent pain following an abdominal trauma with very low energy transfer. Consequently, a pelvic mass occupying the left-lower quadrant was accidentally found during physical and imaging evaluations.
Notably, omental torsion is rarely diagnosed in the preoperative setting, and the possible role of computer tomography and magnetic resonance imaging as pre-operative diagnostic tools is controversial [4]. Thus, surgery is mandatory in order to achieve an adequate diagnosis and prompt treatment. Assuredly, a minimally invasive approach should be preferred if feasible and safe [5, 6]. In the present case, a second line radiological study was not deemed necessary considering the suspected diagnoses (such as ovarian tumor, adnexal torsion or mesenteric neoplasm); and it would not have provided more accurate information on which to base a different treatment strategy. Additionally, a laparoscopic approach would have not allowed a such abdominal mass to be removed.
Lipoblastomas are rare benign tumors of childhood. They are more common in males, with a peak incidence below 3 years of age. Lipoblastomas most commonly occur at the limbs followed by abdomen, head and neck [7, 8]. Occasionally, they can arise as an abdominal mass from the retroperitoneum involving the mesentery or the omentum. When arising in the abdomen, they are usually larger and can cause symptoms of compression or leading to intussusception [7]. Histologically, lipoblastoma is a well-defined entity and differential diagnosis includes lipoma, myxoid liposarcoma and differentiated liposarcoma. To date, only one case of omental lipoblastoma with no signs of torsion has been described [8]. Therefore, to our knowledge, this is the first case in the paediatric literature about an abdominal lipoblastoma arising from the greater omentum and moreover leading to its torsion.
In conclusion, despite omental lipoblastoma is extremely rare in paediatric age, it should be taken into consideration in differential diagnosis when evaluating a child with acute abdominal pain and/or an abdominal mass. Furthermore, when arising from the greater omentum, lipoblastoma might lead to a torsion of the omentum presenting with a specific symptoms.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



