-
PDF
- Split View
-
Views
-
Cite
Cite
A Morera-Grau, E Membrilla-Fernández, A M González-Castillo, A Pelegrina-Manzano, M A Guerrero-Ortiz, C Téllez-Marquès, M J Pons-Fraguero, J Guzmán-Ahumada, M Pera-Román, J J Sancho-Insenser, Caecal volvulus and jejunostomy: challenging diagnostic, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab148, https://doi.org/10.1093/jscr/rjab148
Close - Share Icon Share
Abstract
Caecal volvulus represent the 20–40% of colonic volvulus, being the second most frequent localization. It causes intestinal occlusion symptomatology (nausea, vomiting, abdominal distension). We present a case of 45-year-old women with feeding jejunostomy tube due to connatal anoxia. She arrives at A&E after 12 h of vomits and abdominal pain. The CT scan shows a small intestine dilation that suggested a small intestine volvulus. A laparotomy is performed showing a caecal volvulus, so ileo-cequectomy with primary anastomosis is performed. After several complications, she was discharged after 60 days of hospital stay. Caecal volvulus can be challenging to diagnose by clinic, because it can be hardly differenced from other intestinal occlusion causes. CT scan can be useful to reach the diagnostic and see signs of tissue suffering. In contrast with sigma volvulus, endoscopic treatment has not shown any benefit to solve it.
BACKGROUND
The caecal volvulus is a torsion of this part of large intestine. It represents 20–40% of colon volvulus and is the second most common location after sigmoid colon. It causes about 1–1.5% of intestinal occlusions in adults [1].
Clinically, it causes an inespecific occlusive syndrome.
Definitive treatment is essentially surgical, ranging from cechectomy to right hemicolectomy.
CASE REPORT
A 45-year-old woman is admitted in our hospital because of a 12-h clinic of alimentary vomits and hypoactivity.
Personal antecedents include cognitive disability due to connatal anoxia that causes severe dysphagia, for which she was placed a feeding jejunostomy, a spastic tetraparesia in the left half of the body due to several strokes; structural epilepsy and an emergency laparotomy due to intestinal occlusion when she was 9.
The patient is hemodynamically stable (blood pressure of 132/76 mmHg, heart rate 91 beats/min), a respiratory rate of 16 breaths/min, an O2 saturation of 99% baseline, afebrile. The abdominal examination shows a globular abdomen, diffusely painful on palpation, without signs of peritoneal irritation and with diminished peristalsis.
Fluid therapy, analgesia and antiemetics are administrated. A nasogastric tube and urinary catheter are placed.
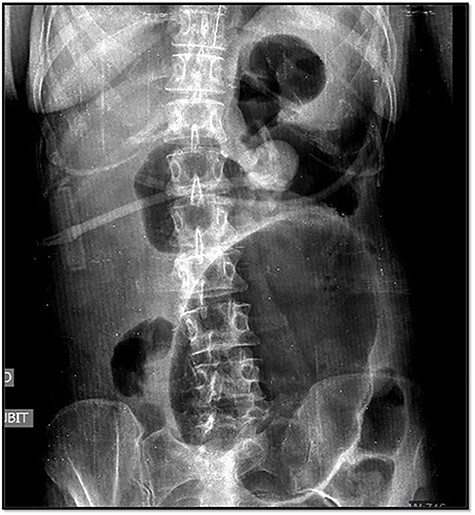
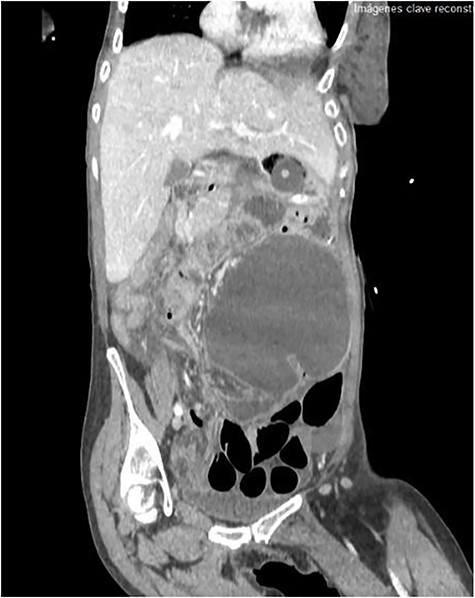
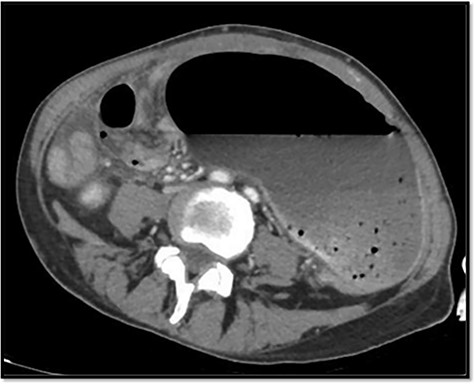
The emergency blood test showed a normochromic and normocytic anemia with an hemoglobin of 10.1 mg/dl and a leukocytosis of 11.150/ul with 70% neutrophils. The abdominal radiography showed a prominent dilation of a small bowel loop. The CT scan reported an 18-cm dilated loop. The main diagnostic suspicion was a small bowel volvulus without signs of ischemia or perforation (Figs 1–3).
With this diagnosis, an emergency laparotomy is performed. It showed a cecum volvulus that compromised 6 cm of distal ileum. The cecum was ischemic, with transmural necrosis. Ileocechectomy was performed including a 15-cm segment of distal ileum. Intestinal transit was reconstructed with mechanical latero-lateral ileo-colic anastomosis with manual reinforcement. The closure of the abdominal wall was performed with a supraaponeurotic prophylactic mesh.
At 24 h after surgery, she presented abdominal distension, pain and anemia with an hemoglobin of 4.9 g/dl. A CT scan reports little blood traces inside the colon without identifying active bleeding, as well as loop dilation suggestive of paralytic ileus. After the transfusion of three packed red blood cells, the patient recovers a hemoglobin of 8 mg/dl. Intraoperative cultures of the peritoneal exudate are negative. Treatment with endovenous cefotaxime (2 g every 6 h) and metronidazole (500 mg every 12 h) is administered for 5 days.
On the ninth post-operative day, she presents a pseudomembranous colitis that responded to oral treatment with Vancomycin for 10 days 500 mg/6 h. She is discharged after 2 months of hospital stay.
DISCUSSION
Caecal volvulus is a rare entity, characterized by a torsion of the cecum, generating a retrograde intestinal dilation and an occlusive syndrome.
Intestinal volvulation is the third cause of obstruction in the large intestine behind neoplastic diseases and diverticulitis. Sigmoid volvulus is the most frequent (75%), followed by cecum (25–40%), transverse colon (1–4%) and splenic flexure (1%). Its annual incidence is 2.8–7.1 cases per million inhabitants [4].
There are three types of caecal volvulus: axial rotation (type 1), the ‘loop’ [axial torsion and inversion (type 2)] and the caecal bascule [the dilated cecum bends on the ascending colon (type 3)]. Type 1 and 2 represent 80% of cecum volvulus.
Volvulus of the cecum can be caused embryologically by an inadequate fixation of the ascending colon or by an absence of fusion of the ascending colon with the lateral peritoneum. Other important predisposing factors are abdominal surgery history; chronic constipation; distal colon obstructions, pregnancy and adynamic ileus [1].
In 50% of cases, a mobile cecum syndrome is described before true volvulation occurs [5], which later resolves after flatulence occurs.
In cases where true volvulation occurs, the symptoms are indistinguishable from those of a small bowel obstruction.
When it comes to intestinal volvulation, the diagnostic and therapeutic speed have a great importance. A volvulus of any type entails a compromise of vascularization due to the rotation of the mesentery, which can lead to necrosis and, therefore, perforation, increasing morbidity and mortality in the patient.
For the diagnosis of this entity, a certain degree of clinical suspicion must be counted since the exploration is common to that of any occlusive process.
The blood analysis of patients with cecum volvulus is also not very specific, reflecting only patterns compatible with intestinal obstruction or sepsis: hydroelectrolyte alterations, leukocytosis, increase in acute phase reactants or alterations in coagulation.
In the abdominal X-ray, one of the three typical signs can be observed: dilation of the cecum, a single air-fluid level in the upper left quadrant of the abdomen or the absence of gas in the colon.
However, abdominal radiographs and soluble contrasts have been relegated in favor of computed tomography. This image has a sensitivity close to 100% and a specificity of 90%. Furthermore, it allows the observation of indirect signs of complications such as necrosis or perforation [3].
In terms of treatment, it differs from volvulus in other segments of the large intestine: cecum volvulus is always a surgical emergency, despite the absence of serious radiological or clinical signs. Even though colonoscopy is the first therapeutic step in other segments of the large intestine, in the case of cecum volvulus its efficacy is less than 30%, so it is not commonly used [3].
The treatment generally requires laparotomy with resection of the ischemic or necrotic segment, and reconstruction of the transit depending on the stability of the patient. Other techniques include cecopexy, or detorsion without posterior fixation, with poorer results in terms of mortality and recurrence [6].
Factors that increase the risk of necrosis in volvulation include a history of cardiovascular disease, chronic kidney disease, hemiplegia and prolonged duration of symptoms [7].
CONCLUSION
Cecum volvulus is a rare pathology, so it can be difficult to diagnose. Clinically, it does not differ from other intestinal obstruction. CT scan is key to determine the etiology of the occlusive condition, as well as to show ischemia and perforation. Definitive treatment is always surgical, using one technique or another depending on the findings.



