-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas Schriener, Stefan Berkhoff, Mohsen Ezzy, Thomas W Kraus, Moustafa Elshafei, Modified laparoscopic toupet fundoplication with fundo-phrenico-pexy, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab136, https://doi.org/10.1093/jscr/rjab136
Close - Share Icon Share
Abstract
This article presents an alternative technique to the common Toupet fundoplication. It is a modern combination of the standard Toupet procedure and an additional fundophrenicopexie of the gastric wrap. In 1963 Toupet first described his technique of a fundoplication for reflux surgery. Over the past years this procedure has been modified and expanded many times. We have learned that the short gastric vessels need to be divided to get the wrap closer and easier around the esophagus. Furthermore, it is likely necessary to perform a balanced hiatoplasty to avoid slippage of the wrap. Our procedure is a modification of the standard Toupet fundoplication, but is extended by fixing the wrap to the anterior wall of the diaphragm. We consider our modification successful and safe in treating gastroesophageal reflux disease in patients with type I/II hiatal hernia and prevent postoperative complications such as dysphagia or slippage of the wrap.
The patient is placed in a beach chair position with legs spread, the upper part of the body is slightly elevated. The right arm is adducted and the left arm is 90° abducted. The operating surgeon stands between the patient’s legs, while the camera operator stands on the patient’s left side.
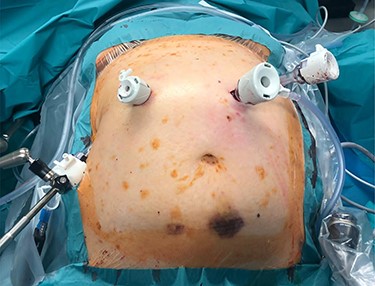
We use four trocars (two 10 mm and two 5 mm) including the optic trocar and a liver retractor system trocar (Fig. 1).
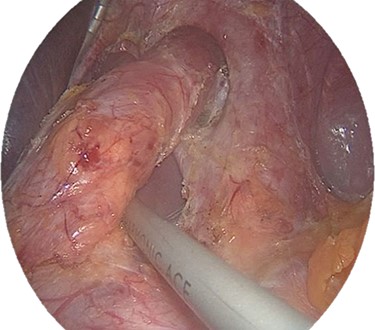
We usually start by dividing the short gastric vessels of the greater curvature of the stomach using ultracision harmonic scalpel (Ethicon). This step requires high precaution because of the possible adhesions to the spleen which can easily be damaged. After dissection of the left diaphragmatic crus, we divide the hepatogastric ligament and phrenoesophageal membrane preserving the hepatic branch of the vagus nerve, as well as the hepatic branches of the left gastric artery. The following step is the identification and dissection of the diaphragmatic pillars and separation of the esophagus from the hiatus. As soon as the right hiatal crus is dissected, the posterior and anterior part of the hiatal window can be prepared. Note that the two vagus nerves are always identified and stay secure to avoid nerval injuries (Fig. 2).
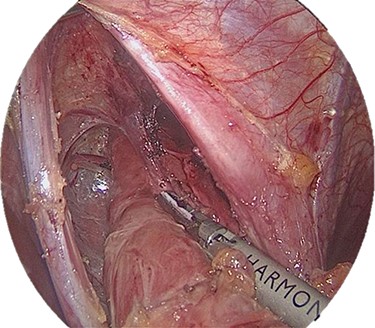
We perform mediastinal circumferential dissection of the lower esophagus for at least 5–6 cm preserving the anterior and posterior vagus nerves and pleura. Both the mediastinal dissection and the removal of hernia sack will create more length of intraabdominal esophagus.
We usually use a tape that is placed around the posterior esophagus for proper traction in order to facilitate further crural dissection and adequate mobilization of the lower esophagus. After the appropriate creation of the intra-abdominal esophagus, the gastroesophageal junction can be fully identified (Fig. 3).
A posterior hiatoplasty is performed by two to three non-absorbable mersilene sutures using the Endo Stitch suturing device (Medtronic). Performing a balanced hiatoplasty by adding anterior sutures can be useful to avoid any stenosis or kinking at the gastroesophageal junction. The hiatoplasty is created over a 10 French bougie kept inside the esophagus throughout the surgery (Fig. 4).
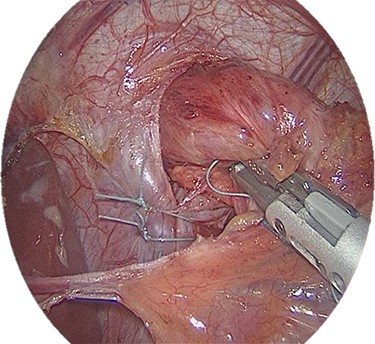
Posterior hiatoplasty (note that the vagal and arterial hepatic branches are preserved).
To create the 270° posterior wrap, sufficient mobilization of the gastric fundus is done and is passed behind the esophagus from left to right. The tailoring of the wrap is controlled by a 10 French esophageal bougie.
The wrap posture is controlled to avoid any twists and torquing.
Then, we start the ‘Fundophrenicopexy’ by anchoring the right part of the fundoplication with two sutures to the anterior diaphragm. Care must be taken because of the close proximity to the pericardium. This step describes a modification of the common toupet and is designed to prevent slippage of the wrap. Further fixations of the wrap and the fundus to the left and right crus are performed. Regardless of the wrap’s anchoring, the hiatal closure can be supported by an additional mesh closure as shown below (Fig. 5).
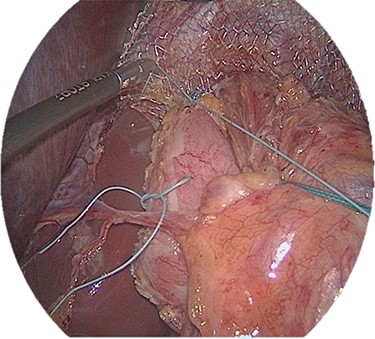
Fixation of the wrap (top fixation to the diaphragm, right and left fixation to the crus and the esophagus).
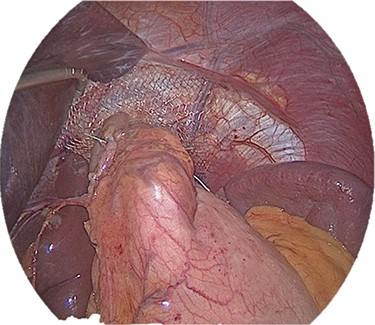
Before finishing the procedure, both parts of the wrap are fixed to the anterior wall of the esophagus. Precautions are taken to avoid any vagal nerve injuries (Fig. 6).
RESULTS
Between December 2019 and November 2020, we have operated on 105 patients with this technique. The mean operative time was 69.5 minutes; no intra-operative complications occurred. The mean post-operative stay was 2.3 days (2–3 days). There were two patients with early dysphagia. In both cases, no further interventions nor any revisional surgerys were necessary.
CONCLUSIONS
This modified method for standardized toupet fundoplication including the fundophrenicopexy is safe and may reduce postoperative dysphagia and the risk for wrap dislocation.
Prospective randomized studies are recommended to investigate and observe the following:
Postoperative dysphagia
Improvement of reflux symptoms
Recurrence rate of the hiatal hernia
General improvement in quality of life
Frequency of proton pump inhibitor intake
CONFLICTS OF INTEREST STATEMENT
None declared.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
Dr Thomas Schriener: literature review, data collection and writing the manuscript.
Dr Mohsen Ezzy: final review.
Dr Mostafa Elshafei: study concept, primary surgeon, review and editing.
Dr Stefan Berkhoff: final review.
Dr Thomas Kraus: final review.
All authors read and approved the final manuscript.
CONSENT
Written informed consent was obtained from the patient for publication with accompanying images.
ETHICS APPROVAL
Not applicable.



