-
PDF
- Split View
-
Views
-
Cite
Cite
Venkiteswaran Muralidhar, An unusual presentation of acute abdomen: infarcted peritoneal cyst-a probable asbestos-related benign cystic mesothelioma, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab129, https://doi.org/10.1093/jscr/rjab129
Close - Share Icon Share
ABSTRACT
This is a report of a rare case of an infarcted pelvic intra-abdominal cyst, having no mesenteric connection presenting as an acute abdomen. The patient had significant asbestos exposure. The cyst was treated successfully by surgical excision. Histopathology showed an infarcted cyst; the lining was destroyed, precluding marker studies. A diagnosis of benign cystic peritoneal mesothelioma (BCPM) was made by excluding other causes of solitary pelvic intra-abdominal cysts. BCPM has been classified as an asbestos-related neoplasm and is usually seen in the pelvis adjunct to the urinary bladder. One-year post-surgery, there was no recurrence. The case report shows that infarcted pelvic mesothelial cysts can present as an acute abdomen and can be treated successfully by total excision with no recurrence.
INTRODUCTION
Infarction of pelvic benign peritoneal mesothelioma (PBPM) has not been reported. These cases may have a history of asbestos exposure [1, 2]. PBPM are rare cases usually situated in the pelvis in association with the urinary bladder [1, 3]. Infected or infarcted intra-abdominal cysts can present as an acute abdomen [4].
CASE REPORT
A 42-year-old male non-smoker and non-alcoholic presented with acute right-sided abdominal pain, vomiting, dysuria and fever. The pain was in the right lower abdomen and aggravated by movement. He had nausea and non-bilious vomiting. He had painful micturition with concentrated urine. He had no prior abdominal trauma or surgery. He had no weight loss, diabetes, hypertension, tuberculosis or pancreatitis. He worked as a construction worker for 15 years. He worked in 8-hour shifts, 6 days a week, throughout the year. His main job was to mix cement with asbestos and erect asbestos sheets. He has been handling asbestos daily for >10 years. Physical examination showed: Heart rate 120 bpm, blood pressure 110/70 mm Hg, temperature 39°C, distension and guarding in the right iliac and umbilical region.
Chest radiology and cardiogram were normal. Sputum was negative for acid-fast bacilli. Lab reports showed: haemoglobin 10.4 g/dl, white blood cell 6400 per microlitre, serum creatinine 0.9 mg/dl, alanine-aminotransferase 16 IU/L, aspartate-transferase 51 IU/L, lipase 149 IU/L, amylase 49 IU/L, serum Na + 129 mmol/L, Glucose 146 mg/dl, partial pressure of oxygen 54 mm Hg. Urine microscopy showed numerous red blood cells.
Abdominal ultrasound showed a well-defined intra-abdominal cyst with clear echoes situated in the pelvis compressing and displacing the urinary bladder to the left. The rest of the organs were normal. There was no free fluid.
Computerized tomography showed a solitary well defined intraperitoneal cyst consisting of fluid showing low attenuation. The wall of the cyst was 1 cm thick, with no contrast enhancement. It was situated in the pelvis compressing the urinary bladder. It had no communication with either the bowel or the urinary bladder. The pancreas was normal, as also the rest of the abdominal organs. There was no ascites (Figs. 1–5). The diagnosis was a large intraperitoneal infected cyst.
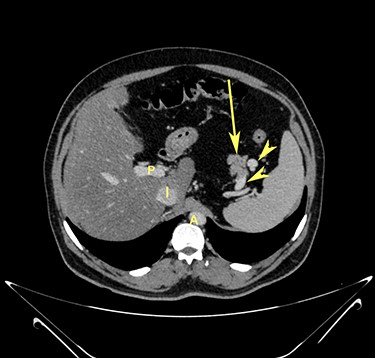
Transverse section image of a contrast-enhanced CT scan of the abdomen at level 1–1 (Fig. 1), showing the pancreas’ normal tail (long arrow). Splenic vessels are labelled using arrowheads.
Transverse section image of a contrast-enhanced CT scan of the abdomen at level 2–2 (Fig. 1), showing the pancreas’ normal head and body (long arrow). The confluence of the splenic vein and portal vein are labelled using arrowheads.
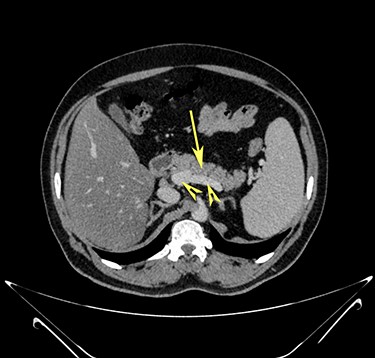
Transverse section image of a contrast-enhanced CT scan of the abdomen at the level 3–3 (Fig. 1), showing a solitary cyst (arrow) with a non-enhancing wall separate from the intestines.

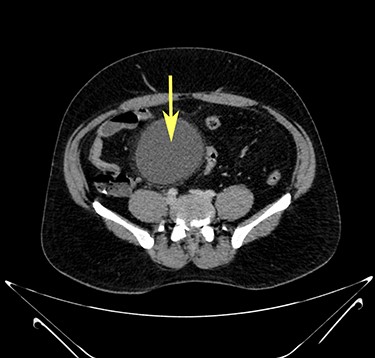
Transverse section image of a contrast-enhanced CT scan of the abdomen at the level 4–4 (Fig. 1), showing a solitary cyst (C) with a non-enhancing wall separate from the urinary bladder (B). Iliac vessels are labelled with arrowheads.
At laparotomy, a sizeable intra-abdominal cyst, free from the mesentery, omentum and mesocolon, was seen occupying the pelvis, compressing the urinary bladder’s superior aspect. There was no connection between the cyst and the anterior abdominal wall, the umbilicus or the urinary bladder (Fig. 6). The wall of the cyst was blackish suggestive of infarction (Figs. 7 and 8). The fluid within the cyst was clear. Complete excision of the cyst was performed. The patient was given third-generation cephalosporins for 3 days. The fluid culture reported no growth of bacteria. The patient showed significant signs of improvement on the second postoperative day. Microscopic haematuria resolved. He was discharged on the 10th postoperative day. He showed no recurrence at 1 year of follow-up.
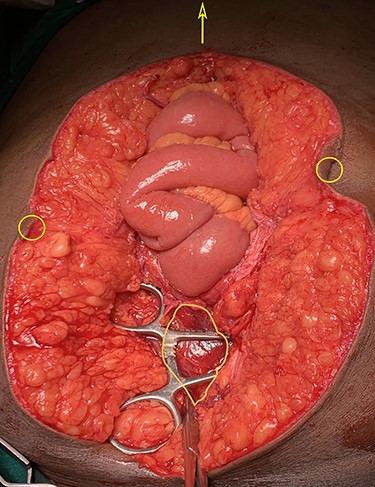
Laparotomy image showing an intraperitoneal cyst in the pelvis (irregular outline), free from the umbilicus (circles) and the intestines. Arrow points towards xiphisternum.
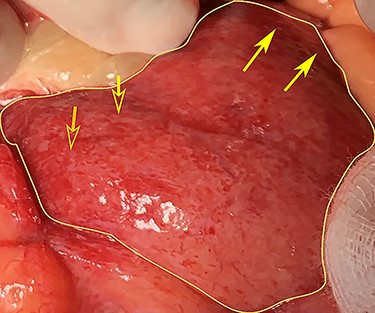
Laparotomy image of the anterior wall of the cyst (irregular outline) showing haemorrhage (open arrows) and infarct (closed arrows).
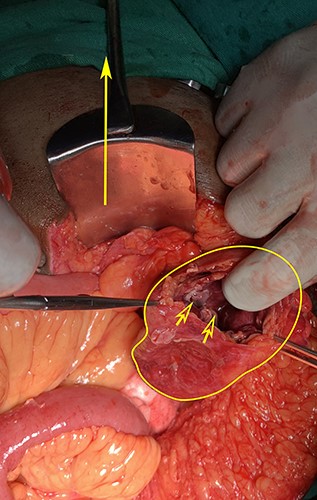
Laparotomy image showing the cyst opened anteriorly (irregular outline), inner aspect of opened cyst showing a blackened gangrenous appearance (open arrows). The filled arrow points to the pubic symphysis.
Histopathology showed cyst wall infarction with infiltration of inflammatory cells, blood vessels and extensive intra-mural bleeds. Few collagen fibres were seen (Fig. 9). Immunohistochemistry could not be done as the epithelial lining was destroyed totally.
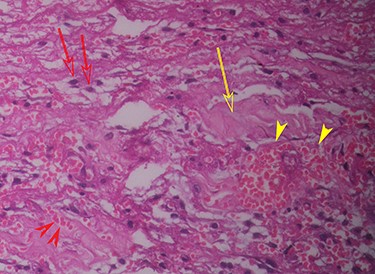
Histopathology (haematoxylin and eosin staining) of the cyst wall (higher magnification) shows haemorrhage (red arrowhead), vascularity (yellow arrowhead), mononuclear inflammatory cells (red arrow) and collagen (yellow arrow).
DISCUSSION
Mesenteric cysts are classified as mesothelial and omental cysts, lymphatic cysts, cysts with solid components (e.g. malignant cysts), infections and infestations (hydatid, tuberculosis and others), pseudocysts (pancreatic and non-pancreatic), enteral, urothelial cysts, teratomas and urachal cysts [5, 6]. The case under study was a solitary cyst free from adjoining structures, having no solid components. Hence, the differential diagnosis of the case includes:
Mesenteric cyst
Lymphatic cyst
Urachal cyst
Pseudocyst
Benign cystic peritoneal mesothelioma (BCPM).
In the absence of communication either with the urinary bladder, umbilicus or the anterior abdominal wall, a urachal cyst can be ruled out [6]. Lymphatic cysts are rarely solitary, may have septa, could insinuate between tissues precluding a complete excision, may have milky chylous fluid or debris, imaging may show enhancement of the cyst wall and histopathology would show clear spaces with lymphatic elements [5, 6]. A pseudocyst is associated with infections or trauma [6]. As there was no evidence of pancreatitis, trauma or prior abdominal surgery, and the enzymes were in the normal range, the imaging and visual examination were normal; a pseudocyst can also be ruled out.
In the study case, there was an absence of connections with either the intestinal or sigmoid mesentery and the omentum, and hence a mesenteric cyst was excluded. Our case was a thick-walled solitary intra-abdominal cyst, whose contents showed clear serous fluid, situated in the pelvis compressing on the urinary bladder that was free from the mesentery, omentum and mesocolon. Our case does not fit into any of the above categories described. Hence, it may be a case of a benign cystic peritoneal mesothelioma (BCPM), with asbestos as a probable cause. Indeed BCPM are rare, situated in the pelvis close to the superior aspect of the urinary [1, 3, 7]. In the absence of the lining, as in our case, immunohistochemistry for mesothelial elements was not possible. If the lining of the cyst is destroyed, the diagnosis may be made from clinical, imaging and operative findings as was reported in a case of a mesenteric cyst [4]. The lining of cysts may also be destroyed, especially if the cyst gets infected. It was suggested that BCPM is a non-neoplastic cyst that has no relation to asbestos exposure and develops probably due to chronic irritation after prior pelvic surgery or pelvic endometriosis [1, 5]. Nevertheless, asbestos exposure has been reported in BCPM [1]. Recently, BCPM has been classified as a neoplastic lesion that could have a causal relation to asbestos and turn into malignancy subsequently [2]. India, the largest consumer of asbestos in the world, has recently reported the first case of asbestos-induced malignant mesothelioma [8].
In the case study, a middle-aged man with significant exposure to asbestos presented as a case of acute abdomen with a solitary infarcted intra-abdominal pelvic cyst, treated successfully with excision asymptomatic after 1 year, was diagnosed as a BCPM by excluding all other possible diagnoses.




