-
PDF
- Split View
-
Views
-
Cite
Cite
Jenny Sohn, Justin S Gundara, Intra-splenic ovarian cystadenoma, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab108, https://doi.org/10.1093/jscr/rjab108
Close - Share Icon Share
Abstract
Splenic cysts are relatively common and usually involve post-traumatic or infective aetiologies. The management of splenic cysts varies in its aetiology, symptomology and size. Surgical intervention is warranted for symptomatic, larger sized cysts > 5 cm and can involve spleen-preserving laparoscopic cyst fenestrations, marsupialization or potentially a splenectomy. In this case report, we review a rare case of an ectopic ovarian cystadenoma presenting as a large recurrent splenic cyst.
INTRODUCTION
Splenic cysts are a relatively common and typically involve post-traumatic or infective aetiologies. Management of splenic cysts relies on its size, infective status and symptomology. Surgical intervention is often warranted for symptomatic, larger cysts > 5 cm. Operative intervention range from spleen-preserving laparoscopic cyst fenestrations or marsupialization to a total splenectomy. We report a rare case of ‘a simple splenic cyst’ which ultimately was shown to be a rare ectopic ovarian serous cystadenoma.
CASE REPORT
A 39-year-old woman presented to our service for review following a failed laparoscopic fenestration of a reported simple large splenic cyst. She possessed no background history of note and was on the oral contraceptive pill. She gave a history of having worsening and progressive left upper quadrant pain over the last 2 years. This had been investigated with ultrasonography, which revealed a large uncomplicated splenic cyst. This had previously been managed with percutaneous aspirations and ultimately a laparoscopic cyst wall fenestration and drainage.
Two weeks following the laparoscopic cyst wall fenestration and drainage, patient re-presented with recurrent left upper quadrant pain. She was referred to our service when repeat ultrasound imaging showed re-accumulation of the cyst. Given the size of the cyst and previous interventions, an open splenectomy was performed following immunization. Operation was completed without complication and the patient made an uneventful recovery. Figure 1 shows the macroscopic splenectomy specimen.

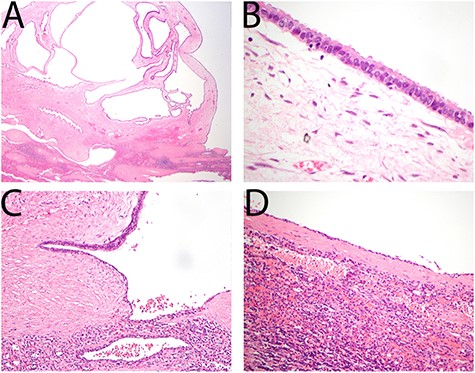
(A) Cyst wall demonstrated typical features of ovarian type serous cystadenoma composed of bland serous epithelial cells overlying ovarian type stroma. (B) Epithelial cells show typical serous features including cuboidal cytology and ciliation. (C) Ovarian type stroma merging with areas of splenic epithelial cyst with attenuation of the epithelium and loss of cilia. (D) Majority of the cyst shows typical features of a splenic epithelial cyst.
At pathologic evaluation, it was evident that 80% of the spleen was occupied by a 100 × 100 × 70-mm cyst. Microscopy demonstrated the presence of an ovarian type, serous cystadenoma. Typical ciliated serous epithelium overlying an ovarian type stroma was evident as shown in Fig. 2 (CD10 positive). Otherwise, the immune-profile was typical for an ovarian type serous cystadenoma, being positive for CK7, WT1, BerEP4, BAP1, oestrogen receptor, progesterone receptor and Pax8.
DISCUSSION
Ovarian serous cystadenomas (OSC) are the commonest type of ovarian epithelial tumours [1] and largely occur unilaterally. They are characterized by epithelium resembling that of the fallopian tube or surface epithelium of ovaries. Ciliated cells are universally found in benign serous tumours [2]. If ectopic, OSC’s are para-ovarian in location. Intra-splenic ectopia is an extremely rare site for OSC and has not been reported previously.
Clinically, OSC’s present most commonly with abdominal or pelvic pain and peak in pre-menopausal women between the second and fourth decade of life [3]. Prior studies have shown that cysts may grow to a relatively large size before becoming symptomatic (mean 5.7-cm diameter) [3].
First line investigations typically involve imaging. On ultrasound, characteristic appearance involves a unilocular cystic adnexal lesion with an absence of papillary projections on regular surfaces [4, 5]. Similarly, on computed tomography, OSC’s show a thin, regular walled unilocular cystic mass with homogenous attenuation and an absence of endocystic or exocystic growths [6]. On magnetic resonance, the cyst wall may enhance following contrast (e.g. gadolinium) [6]. Imaging should be supplemented by tumour markers [7] including CA-125 as ~20% of borderline epithelial tumours appear as ‘simple cysts’ on imaging alone.
The paucity of data on non-parasitic splenic cysts limits the development of a defined management algorithm. Overall recommendations for non- symptomatic splenic cysts < 5 cm remain conservative [8] with serial imaging surveillance. Laparoscopic methods have been suggested as first line for symptomatic cysts. It has advantages of reduction in postoperative pain, length of hospitalization, improved cosmesis and preservation of splenic function [9]. Total splenectomy, as in this case report, is indicated when minimally invasive surgical techniques or operations like partial splenectomy have failed [8]. Given the rare nature of the presenting case, a referral to a gynaecologist is necessary to investigate potential further involvement of para-ovarian organs. Generally, benign cystadenomas offer good prognosis [10].
In conclusion, when establishing a list of differential diagnosis for splenic cysts and masses, clinicians should be alert to the rare possibility of cystadenoma/cystadenocarcinoma with ovarian subtypes as demonstrated in this case.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
Serov, S. F, Scully, RE, Sobin, LH & World Health Organization. WHO Epithelium International Histological Classification of Tumours: Histological typing of ovarian tumours. Geneva, World Health Organization, 1973.



