-
PDF
- Split View
-
Views
-
Cite
Cite
Akshat T Parekh, Keith Diamond, Monty Littlejohn, Hamid Ehsani-Nia, Chris Amro, Amyand’s hernia complicated with appendicitis: an interval approach with transabdominal laparoscopic appendectomy and laparoscopic hernioplasty—a case report, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjaa499, https://doi.org/10.1093/jscr/rjaa499
Close - Share Icon Share
Abstract
Amyand’s hernia is a rare classification of inguinal hernia where the vermiform appendix is located within the hernial sac. This case report discusses a patient presenting with abdominal and groin pain shown to be an Amyand’s hernia complicated by acute appendicitis on computed tomography. The patient was treated with a two-stage approach, involving transabdominal laparoscopic appendectomy and elective laparoscopic hernioplasty after recovery. As some controversy exists regarding the timing of appendectomy and hernioplasty, we examine the benefits of the interval approach in the reduction of postoperative infection risk compared with a concurrent approach in patients presenting with Amyand’s hernia complicated by appendiceal inflammation.
INTRODUCTION
Amyand’s hernia is defined as an inguinal hernia with the presence of the vermiform appendix within the hernial sac. Amyand’s hernia is named after Dr Claudius Amyand who performed the world’s first successful appendectomy on an 11-year-old boy with an inguinal hernia combined with an acutely inflamed appendix [1]. The incidence of Amyand’s hernia is varied in literature, ranging from 0.19% to 1.7% of reported hernia cases [2]. The incidence of appendicitis within an inguinal hernia is even lower, with an estimated rate of 0.07–0.13% [3]. The best course of action for surgical treatment of an Amyand’s hernia is still up for debate. This case report discusses the successful diagnosis and management of an Amyand’s hernia complicated with appendicitis, using a two-stage approach.
CASE REPORT
An 81-year-old male with a past medical history of childhood repair of cardiac septal defect presented to our emergency department (ED) with a two-day history of vague abdominal pain that migrated to his right groin with an associated non-reducible right groin mass. The non-reducible groin mass persisted, and his pain progressed that prompted him to come to the ED. Clinical examination revealed a firm, tender and irreducible right inguinal mass. The remaining clinical and laboratory tests were normal. Contrast-enhanced computed tomography (CT) of the abdomen and pelvis was performed. CT presented an acute appendicitis within a right inguinal hernia and a dilated appendix, measuring 13 mm in diameter and demonstrated periappendiceal fat stranding with no evidence of rupture (Figs 1–3). Patients’ history, physical exam and imaging findings were consistent with the preoperative diagnosis of an Amyand’s hernia with acute appendicitis. It was determined the patient will require operative intervention.
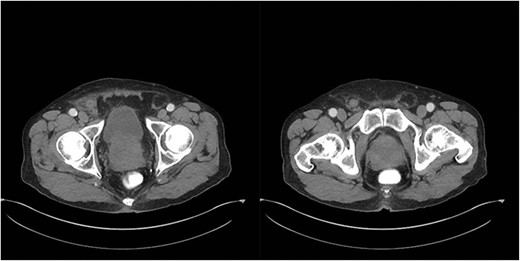
Axial CT abdomen with oral contrast showing a dilated appendix periappendiceal fat stranding within a right inguinal hernia and no evidence of rupture.

Coronal CT abdomen with oral contrast showing a dilated appendix periappendiceal fat stranding within a right inguinal hernia and no evidence of rupture.
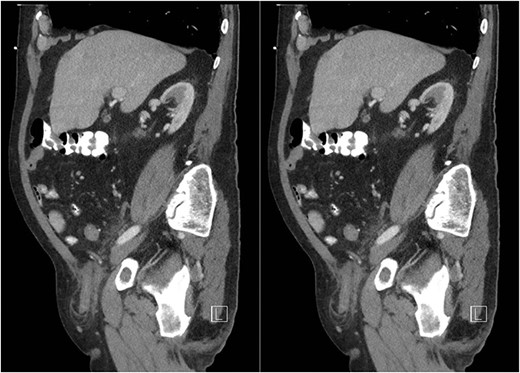
Sagittal CT abdomen with oral contrast showing a dilated appendix periappendiceal fat stranding within a right inguinal hernia and no evidence of rupture.
A diagnostic transabdominal laparoscopy was performed to visualize the right lower quadrant and inspect the hernia. Using a combination of external pressure in the groin and retraction internally after placing two additional 5-mm ports in the suprapubic region and left lower quadrant, the team was able to retract the appendix out of the hernial sac. The appendix appeared to be inflamed, though it was neither perforated nor gangrenous. Laparoscopic appendectomy for acute appendicitis was performed. Pathological examination confirmed acute appendicitis with focal necrosis. After further visualizing the hernia defect, the team determined the patient would best benefit from an elective hernia repair in the future to avoid infectious complications of immediate mesh repair. The postoperative course was uneventful, and the patient was discharged the following day. The patient was lost to follow-up before the completion of the hernioplasty.
DISCUSSION
The clinical image of Amyand’s hernia resembles that of an incarcerated hernia; thus, it is difficult to diagnose clinically [4]. Previous reports show that the diagnosis was typically made intraoperatively [3, 4]. However, the use of CT and ultrasound allows for preoperative diagnosis and facilitates a shift in surgical approach [5]. The inflammatory status of the appendix in the hernial sac helps dictate the surgical option [5]. Losanoff and Basson [6] created a classification and staging system for Amyand’s hernia with an algorithm to help guide management. According to these authors, Amyand’s hernia can be divided into four subtypes as shown in Table 1. Further modification, known as the Rikki modification, adds a fifth type of Amyand’s hernia described as an incisional hernia through which the vermiform appendix protrudes [7]. Based on Losanoff and Basson, our patient had a Type 2 Amyand’s hernia, due to the concominant inflamed appendix.
Subclassifications of Amyand’s hernia as described by Losanoff and Basson [6]
| Classification . | Description . |
|---|---|
| Type 1 | Amyand’s hernia with a normal-appearing appendix in the inguinal sac |
| Type 2 | Amyand’s hernia with inflamed appendix |
| Type 3 | Amyand’s hernia with a perforation of the vermiform appendix |
| Type 4 | Amyand’s hernia with complicating intra-abdominal pathology (e.g. abscess or malignancy) |
| Classification . | Description . |
|---|---|
| Type 1 | Amyand’s hernia with a normal-appearing appendix in the inguinal sac |
| Type 2 | Amyand’s hernia with inflamed appendix |
| Type 3 | Amyand’s hernia with a perforation of the vermiform appendix |
| Type 4 | Amyand’s hernia with complicating intra-abdominal pathology (e.g. abscess or malignancy) |
Subclassifications of Amyand’s hernia as described by Losanoff and Basson [6]
| Classification . | Description . |
|---|---|
| Type 1 | Amyand’s hernia with a normal-appearing appendix in the inguinal sac |
| Type 2 | Amyand’s hernia with inflamed appendix |
| Type 3 | Amyand’s hernia with a perforation of the vermiform appendix |
| Type 4 | Amyand’s hernia with complicating intra-abdominal pathology (e.g. abscess or malignancy) |
| Classification . | Description . |
|---|---|
| Type 1 | Amyand’s hernia with a normal-appearing appendix in the inguinal sac |
| Type 2 | Amyand’s hernia with inflamed appendix |
| Type 3 | Amyand’s hernia with a perforation of the vermiform appendix |
| Type 4 | Amyand’s hernia with complicating intra-abdominal pathology (e.g. abscess or malignancy) |
When conducting an appendectomy for in Amyand’s hernia complicated by acute appendicitis with or without perforation, literature suggests utilizing the laparoscopic approach for diagnostic and therapeutic purposes [5, 8]. The laparoscopic transabdominal approach allows for better visualization and management of the entire appendix and its base without enlarging the hernia defect or weakening the anatomical structures surrounding it [5, 8].
On the other hand, controversy exists regarding the method of hernia repair regarding the use of mesh when an inflamed or perforated appendix is present in Amyand’s hernia due to the concern of surgical site infections when performing immediate mesh hernioplasty [2, 3, 5]. In a case series of six appendiceal femoral hernias by Priego et al. [9], wound infection occurred in half of the cases complicated by acute appendicitis where mesh was used. Thus, in order to reduce infection risk, many surgeons opt for simultaneous hernia repair using a Bassini’s suture repair in Amyand’s hernias associated with appendiceal inflammation [2, 3]. However, suture repairs are generally associated with a seven times higher recurrence rate than mesh hernioplasty for inguinal hernias [10]. Few cases of Amyand’s hernia have been treated with simultaneous appendectomy and mesh hernia repair but required significant consideration for infection prevention involving a combination of perioperative antibiotics, copious irrigation and washouts or drain placement [2]. However, introduction of prosthetic material into contaminated sites can trigger an increased inflammatory response and serve as nidus for infection [2]. Thus, in order to best minimize the surgical site infection risk, the team decided to take an interval approach and delay laparoscopic mesh hernioplasty until after the resolution of the localized inflammation following the appendectomy.
In conclusion, our patient had a Type 2 Amyand’s hernia, which was managed with a two-stage approach involving a transabdominal laparoscopic appendectomy with elective laparoscopic mesh hernioplasty deferred until after recovery from the appendectomy. This method combines the benefit of increased repair strength associated with mesh hernioplasty while avoiding the infection risks associated with prosthetic mesh placement in a contaminated environment.
CONFLICT OF INTEREST STATEMENT
None declared.



