-
PDF
- Split View
-
Views
-
Cite
Cite
Tia Morosin, M Shella De Robles, Andrew Still, Duodenal diverticulum at the site of the major papilla may be a risk factor for biliary stent migration, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab079, https://doi.org/10.1093/jscr/rjab079
Close - Share Icon Share
Abstract
Stent migration is a well-documented complication following biliary stent insertion. The majority of cases demonstrate passage through the bowel without incident; however, migration may also result in complications, including bowel obstruction or perforation requiring urgent intervention. Risk factors for stent migration comprise of disease pathology as well as stent characteristics including dimension, material and number. Although duodenal diverticulae has been noted as a risk factor for duodenal perforation or obstruction post stent migration, it has yet to be implicated as a contributor to migration itself. Here, we present an unusual case of ileal obstruction secondary to biliary stent impaction, in which the presence of a duodenal diverticulum may be considered a viable risk factor for stent migration.
INTRODUCTION
Endoscopic biliary stent placement is frequently utilized for the management of benign and malignant obstructive biliary pathology. Although a common minimally invasive procedure, it is not without its complications. Of particular interest is stent migration, occurring in up to 10% of patients with risk factors including disease pathology and stent characteristics [1, 2]. Although the majority of migrated stents pass throughout the bowel and are excreted naturally, this passage may also result in complications, including bowel obstruction and perforation requiring urgent intervention [2–4]. To our knowledge, duodenal diverticulum has yet to be proposed as a risk factor for stent migration, and while bowel obstruction may result, it is a rare occurrence in the ileum. Here, we present a rare case of biliary stent migration to the proximal ileum, resulting in a small bowel obstruction requiring surgical intervention, in a patient with a duodenal diverticulum.
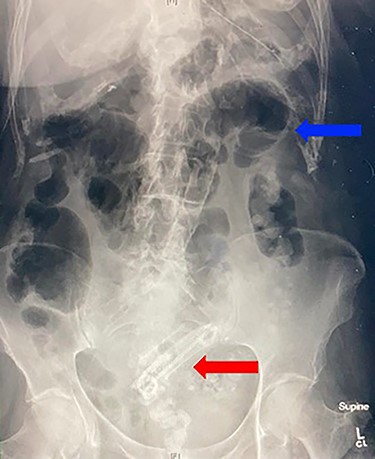
Abdominal X-ray demonstrating projection of biliary stents in the pelvis (red arrow) and multiple air fluid levels suggestive of a small bowel obstruction (blue arrow).
CASE REPORT
A 90-year-old female presented to the hospital for small bowel obstruction requiring surgery. Six months prior, she underwent an endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and insertion of side-by-side straight plastic stents followed by a laparoscopic cholecystectomy for cholangitis secondary to choledocholithiasis. The stents were to be removed 6 weeks post cholecystectomy; however, the procedure was delayed for 5 months due to significant deconditioning requiring prolonged physical rehabilitation. During the repeat ERCP, there were concerns for a biliary mucosal tear resulting in prophylactic insertion of two covered metal biliary stents with two plastic biliary stents in situ. She had an unremarkable hospital admission and was sent home the following day. Two weeks after the repeat ERCP, she presented to the emergency department with colicky abdominal pain, distention and bilious vomiting. Abdominal examination demonstrated a markedly distended abdomen with periumbilical tenderness on palpation. An abdominal X-ray revealed projection of the biliary stents in the pelvis (Fig. 1), with an abdominal computed tomography scan confirming the migration of stents to the small bowel resulting in a small bowel obstruction (Fig. 2A–C). An emergency mini-laparotomy was performed revealing seropurulent ascites and palpable biliary stents obstructing the proximal ileum causing upstream dilatation. A small enterotomy was performed, all four stents were retrieved (Fig. 3A–C) and the enterotomy was closed with interrupted full-thickness repair using 4.0 polydioxanone sutures. The patient had a slow progression due to prolonged ileus and was discharged from the hospital after 2 weeks.
DISCUSSION
Complications from biliary stent insertion may be short or long term and include pancreatitis, cholangitis, haemorrhage, perforation, occlusion, fracture, fistula formation and in the current case migration [1, 5, 6]. Stent migration can be broadly classified as proximal or distal, the duodenum being the most common site [1–3]. Benign biliary disease is associated with greater risk of migration due to the reduction in inflammation and oedema following treatment allowing for movement of the stent, compared with malignant disease, which results in ongoing inflammatory processes helping maintain the stent position [1, 3, 6]. Papillary stenosis has also been identified as a risk for migration; however, there is reported inconsistency regarding the risk posed by sphincterotomy [1, 4, 5]. Stent characteristics also contribute to the risk of migration. Straight stents in particular have been associated with increased risk of migration and perforation compared with pigtail stents [1, 7]. Shorter stents (<7 cm) and those with larger diameters (12French) have similarly demonstrated an increased risk of migration [2, 4]. In addition, the insertion of a single large stent compared with multiple smaller stents may potentially be associated with increased risk of migration [1]. In the present case, multiple stents were inserted, with a combination of covered metal and plastic pigtail stents, all of which should have decreased the patient’s risk of stent migration. Interestingly, the side-by-side straight plastic stents initially inserted for management of cholangitis were also seen to be migrating into the duodenum on stent retrieval, with the proceduralists noting that the major duodenal papilla resided adjacent to a duodenal diverticulum (Fig. 4). Duodenal diverticulum is commonly an incidental diagnosis demonstrated during ERCP, and its presence in the duodenum is similarly associated with bleeding, infection, biliary obstruction and perforation [8, 9]. The adjacent diverticulum may interfere with the normal emptying mechanism of the ductal systems, predisposing patients to biliary obstruction and stent migration. This case suggests that despite using favourable materials to minimize migration, the presence of duodenal diverticulae may in itself be a risk for stent migration. We acknowledge this finding may just be fortuitous and that the stent migration may have been caused by previous manipulation and sphincterotomy in our patient, but we hope that other authors can build on this observation. To our knowledge, this is the first case to suggest that a duodenal diverticulum adjacent to the site of the major papilla is a risk factor for biliary stent migration. Most cases of migration pass through the bowel without incidence; however, it also carries a risk of bowel perforation and obstruction [1, 3]. The incidence of stent migration and impaction in the small bowel is not well documented. Common sites of obstruction occur where there is fixation of the bowel, typically proximal to the ligament of Treitz or at sites of irregularities, including hernia and colonic diverticulae, neither of which were present in the current case [1, 7]. Treatment of stent migration depends on the site of stent migration and impaction. Endoscopic retrieval may be utilized where the stent resides within the duodenum and there are no concerns for perforation; however, prompt surgical intervention should not be delayed in cases of perforation or obstruction [1, 3]. In the current case, endoscopic intervention was not possible due to the number of stents, position within the ileum and presence of a small bowel obstruction requiring urgent surgical intervention. Duodenal diverticulum may present a new risk factor for stent migration. A high index of suspicion for the consequences of migration is required in any patient presenting with obstructive symptoms and a history of biliary stents to ensure prompt intervention.
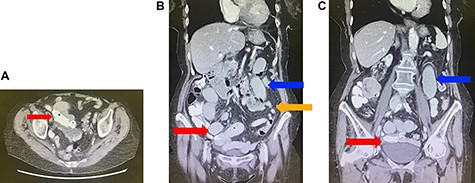
(A) Axial view of computed tomography (CT) of the abdomen demonstrating migration of the biliary stents into the small bowel (red arrow). (B) Coronal view of CT of the abdomen demonstrating migration of the biliary stents into the small bowel (red arrow), with dilated (blue arrow) and collapsed (orange arrow) loops of small bowel suggestive of a small bowel obstruction. (C) Coronal view of CT of the abdomen demonstrating migration of the biliary stents into the small bowel (red arrow) and dilated loops of small bowel (blue arrow).
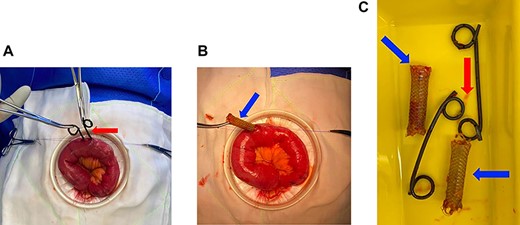
(A) Enterotomy in proximal ileum demonstrating removal of two plastic pigtail stents (red arrow). (B) Enterotomy in proximal ileum demonstrating removal of a covered metal stent (blue arrow). (C) Stents post removal, two plastic pigtail stents (red arrow) and two covered metal stents (blue arrows).
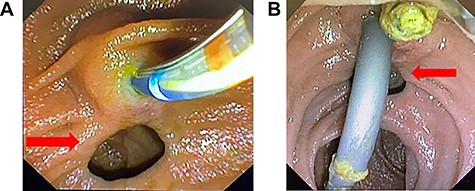
(A) ERCP images demonstrating the duodenal diverticulae (red arrow) at the site of the major duodenal papillae. (B) ERCP images demonstrating the duodenal diverticulae (red arrow) at the site of the major duodenal papillae.



