-
PDF
- Split View
-
Views
-
Cite
Cite
Bruno M Chan Chin, Muhammad Aakif, Ata U Khan, Post-operative abscess in inguinal hernial sac—case report of an unusual complication of perforated acute appendicitis, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab061, https://doi.org/10.1093/jscr/rjab061
Close - Share Icon Share
Abstract
Acute appendicitis is a common condition, with a lifetime risk of 7–8%. Common complications of surgical management include bleeding, bowel injury, residual abscess formation and post-operative ileus. This is a rare case of a 50-year-old male who underwent laparoscopic converted to open appendicectomy for perforated acute appendicitis, with a complication of post-operative fluid collection that extended into the right inguinal hernia sac.
INTRODUCTION
Acute appendicitis is the most common abdominal surgical emergency, with a worldwide lifetime risk of 7–8% [1]. It is predicted that 16% of the population in developed countries will undergo an appendicectomy in their lifetime for possible appendicitis [2], and in the UK, it is estimated that there are 35 000 appendicectomies per year [3]. Common complications related to the procedure include wound infection, bleeding, damage to local structures or post-operative ileus [3]. Below is a case of an unusual post-operative complication of perforated acute appendicitis, a collection in the right inguinal hernia sac.
CASE PRESENTATION
A 50-year-old gentleman presented to the emergency department complaining of a 3-day history of central abdominal pain that migrated to the right iliac fossa, associated with nausea, anorexia and constipation. This was on the background history of bipolar disorder and hypertension. On examination, he was alert, oriented and his vital signs were normal. His abdomen was tender in the right iliac fossa associated with guarding, but no rebound tenderness, Rovsing’s negative, Obturator negative, Psoas negative. No masses were seen or felt. Initial laboratory work demonstrated white blood cell 20.2 × 109/L (neutrophil 19 × 109/L), haemoglobin 14.4 g/dl, urea 9.5 mmol/L, liver function tests (LFT) normal, C-reactive protein 20.1 mg/L and the electrolytes were normal. A computed tomography (CT) of the abdomen and pelvis was performed, which showed a dilated thickened appendix, with periappendiceal fat stranding, consistent with acute appendicitis (Fig. 1).


CT of the abdomen and pelvis demonstrating a fluid collection/abscess extending into a right inguinal hernia sac in (A) coronal (B) sagittal and (C) apical planes.

CT of the abdomen and pelvis demonstrating a reduction in size of the fluid collection/abscess in the inguinal hernia sac in (A) coronal (B) sagittal and (C) apical planes.
While waiting for the surgical intervention, he developed an episode of fever (temperature of 38.9°C), with a respiratory rate of 20 breaths per minute, SpO2 96% on room air, blood pressure 125/82 and heart rate 86 bpm. The sepsis protocol was activated, blood cultures were taken, and he was started on co-amoxiclav and metronidazole intravenously (IV). These blood cultures were positive for gram-positive bacilli, sensitive to the antimicrobials he was already on.
He underwent a laparoscopic appendicectomy, which was converted to open because the appendix was located at a retro-ileal position and the tip of the gangrenous appendix was stuck deep into the ileal mesentery. It was found that the appendix was perforated in the middle with pus and faecal content in the peritoneal cavity. Open lower midline laparotomy was performed, and the appendix was removed piecemeal, the base was normal and ligated using vicryl 2/0 endoloops. The peritoneal cavity was thoroughly washed using 3 L of warm saline. A Robinson drain 21F was placed in the pelvis, and the abdomen was closed with 2 polydioxanone suture (PDS) loops, skin clips and a honeycomb dressing.
Post-operatively, he was managed with IV fluids, adequate analgesia and triple antibiotics (co-amoxiclav, metronidazole and gentamicin), chest physiotherapy and mobilization. The drain was removed on day 3 post-operatively.
He had ongoing episodes of fever (38.1, 38.8 and 38.5°C) on days 3 and 4 post-operatively, so his antibiotics were escalated to piperacillin/tazobactam and metronidazole, according to microbiologist advice. However, on day 5 post-operation, he was still complaining of a severe tenderness on the right iliac fossa, associated with guarding, he was diaphoretic and febrile and clinical examination showed a tender lump in the right inguinal region. A CT of the abdomen and pelvis was performed to assess for a deep-seated collection, and it showed post-operative changes in the right lower quadrant at the site of recent appendicectomy, with small foci of poorly encapsulated fluid in the right lower quadrant with a further more well-defined 7 cm fluid collection/abscess extending from the right lower quadrant into a right inguinal hernial orifice and extending into the hernia sac (Fig. 2).
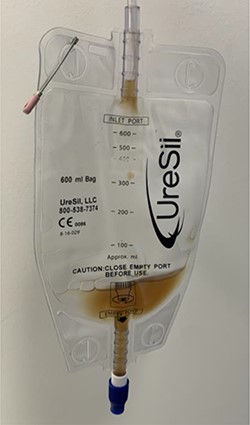
This collection was drained under ultrasound guidance, and a pigtail catheter was left in situ for 1 week. The patient progressively recovered. A repeat CT of the abdomen and pelvis after a week demonstrated a reduction of the collection (Fig. 3).
The patient was discharged with the pigtail drain in situ and reviewed after 1 week in the outpatient clinic. He was clinically well, with no pain in the right iliac fossa and no tenderness on examination. The drain was removed (Fig. 4). An appointment was made to repair the right inguinal hernia with a mesh in a future date.
DISCUSSION
Since the first report of an endoscopic approach to appendicectomy in 1983 [4], the popularity for minimally invasive surgery has increased and it is currently considered to be a safe and effective approach. A recent meta-analysis showed that it leads to a reduction in post-operative pain, fewer surgical wound infections, shorter hospital admission and less overall post-operative complications [5]. However, conversion to open appendicectomy may be required in some patients, in ~10% of cases, most commonly due to inflammatory adhesions that make it technically challenging to continue with laparoscopy or a friable perforated appendix where there is risk of leaving pieces of appendix behind [6].
Post-operative abscess formation complicates between 14.8 and 20% of perforated appendicitis [7]. The risk of abscess formation does not differ among techniques used (open or laparoscopy) [8] and it can be reduced by a thorough peritoneal lavage [2, 9]. In our case, presence of an intact processus vaginalis led to the collection in the inguinal canal complicating post-operative recovery. To date, there are a few case reports of a periappendicular abscess complicating an Amyand’s hernia, which is the presence of the appendix in the hernial sac [10]. However, this case was unusual, as a fluid collection developed into the hernia sac post-operatively.
CONCLUSION
We presented a very rare case of a fluid collection that extends into a right inguinal hernia sac, as a complication of appendicectomy for perforated acute appendicitis.
PATIENT CONSENT
A fully informed consent to publish this case report was obtained from the patient.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



