-
PDF
- Split View
-
Views
-
Cite
Cite
Krystal Dinh, Lucy Manuel, Kalpa Perera, Thomas Daly, A staged hybrid approach to an aberrant right subclavian artery with symptomatic Kommerell’s diverticulum, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab044, https://doi.org/10.1093/jscr/rjab044
Close - Share Icon Share
Abstract
Aberrant right subclavian is a rare anomaly presenting in 0.3–3.0% of the population. Kommerell’s diverticulum is an aneurysm associated with this phenomen; data relating to its incidence is sparse. Currently there are no well-established guidelines for the treatment of Kommerell’s diverticulum, limitation being the rare occurrence of disease and heterogenous population with disease presentation. This case report illustrates a novel approach to the repair of a symptomatic Kommerrel’s diverticulum with severe coronary disease. Management should be tailored on a case by case basis to the individual patient.
INTRODUCTION
Kommerell’s diverticulum is an uncommon vascular anomaly resulting from anomalous aortic arch development [1]. Due to the rare occurrence, well-established guidelines are not available to aid in management decision making. We describe a case of a symptomatic Kommerell’s diverticulum from an aberrant right subclavian artery with concurrent coronary artery disease, which required several staged multidisciplinary procedures.
CASE REPORT
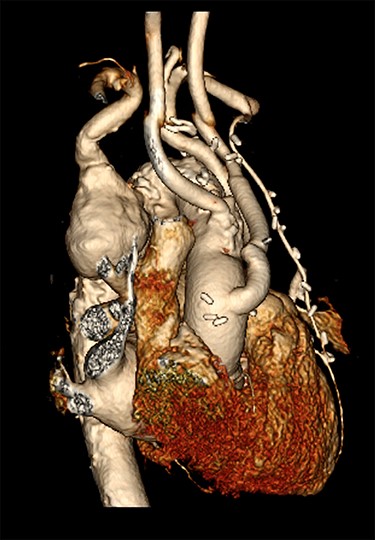
A 78-year-old male presented with sudden onset tearing chest pain with radiation to the back and associated dyspnoea and dysphagia. This was on a background of ischaemic heart disease, hypertension, hypercholesterolaemia and previous small bowel resection for neuroendocrine mesenteric malignancy. He was an ex-smoker with no personal or family history of connective tissue disorders. On computed tomography angiography (CTA) he was found to have an aberrant right subclavian artery (SCA), coursing posterior to the trachea and oesophagus, with an associated 4.4 cm Kommerell’s diverticulum (Fig. 1). Imaging also illustrated tracheal stenosis and oesophageal compression. A coronary angiogram demonstrated severe double vessel coronary artery disease. A staged procedure with aortic arch debranching and coronary artery bypass grafting (CABG), followed by a thoracic stent graft and amplatzer plug to address the Kommerrel’s Diverticulum was planned.

Computed tomography (CT) reconstruction illustrating Kommerell’s diverticulum and an aberrant right subclavian artery.
CT reconstruction illustrating a debranched left common carotid artery and subclavian artery with double coronary artery bypass graft (left internal mammary artery to left anterior descending, and saphenous vein T graft to obtuse marginal artery).
The initial procedure, performed via a median sternotomy, involved debranching the left common carotid artery (CCA) and left SCA with simultaneous double vessel CABG (left internal mammary artery to left anterior descending, and saphenous vein T graft to obtuse marginal artery) (Fig. 2). This provided a sufficient landing zone for a thoracic aortic stent graft. His post-operative recovery was complicated by atrial fibrillation, hospital acquired pneumonia and delirium requiring reintubation for severe agitation. The patient was discharged home following rehabilitation with a plan to perform the second stage of the repair as a semi-elective procedure.
Given the index CTA illustrated a non-dominant right vertebral artery, with known collateralisation of the blood supply to the arm, a decision was made not to perform a carotid subclavian bypass, unless the patient illustrated vertebrobasilar insufficiency. At the second procedure 7 months later, the right subclavian artery was plugged with an Amplatzer (Saint Jude) plug and a GORE (Flagstaff, Arizona) C-TAG stent graft was deployed via femoral access to exclude the Kommerell’s diverticulum and maintain patency of the thoracic aorta (Fig. 3). The post-operative course was uneventful, and the patient was discharged home. There was no immediate noticeable difference in swallowing, however his breathing had improved.

Angiography illustrating Kommerell’s diverticulum before and after deployment of Amplatzer plug (A) to right subclavian and thoracic aortic stent graft (B).
At routine, 4 weeks follow-up the patient reported pre-syncopal episodes with associated right-hand paraesthesia, likely explained by vertebral-basilar insufficiency. A right carotid-subclavian artery bypass with 6 mm ring reinforced polytetrafluoroethylene (PTFE) (GORE PROPATEN) was performed to correct this. There were no immediate post-operative complications and the patient was discharged home. At 6-week follow-up, he had improved right hand symptoms with no further pre-syncopal episodes and had improved swallow.
DISCUSSION
Kommerell’s diverticulum, most often associated with dilatation at the origin of an aberrant subclavian, is an uncommon vascular anomaly resulting from anomalous aortic arch development [1]. Kommerell’s diverticulum and aberrant take off of the SCA results from incomplete regression and is a remnant of the fourth primitive dorsal arch [2]. Due to the rare occurrence, well-established guidelines are not available to aid in management decision making [3]. Aberrant right subclavian is a rare aortic arch anomaly presenting in 0.3–3.0% of the population [4]. Kommerell’s diverticulum is usually an incidental finding, however, patients can present with symptoms, most notably dysphagia lusoria, chest pain and dyspnoea [2]. This case report illustrates a novel approach to the repair of a symptomatic Kommerell’s diverticulum with severe coronary disease.
Given the scarce evidence base, mostly consisting of small case series and reports, management should be tailored on a case by case basis to the individual patient. Surgical treatment remains controversial and should be considered if patients are symptomatic with some suggestion of a Kommerell’s diverticulum of >3 cm being an indication for operating in a low-risk patient [1]. Open, endovascular and hybrid procedures have all been successfully performed with acceptable rates of morbidity and mortality [2]. This suggests that the choice of treatment should be tailored to the patient-specific anatomy, associated morbidity and expertise of the treating surgical team [5].
The need to preserve SCA in the setting of standard thoracic endovascular aortic repair for degenerative aneurysmal disease or type B thoracic dissection is not essential [6]. However, in this instance the decision to delay the revascularisation of the right subclavian in this case lead to vertebrobasilar insufficiency, a known complication of this procedure.
CONFLICT OF INTEREST STATEMENT
None declared.



