-
PDF
- Split View
-
Views
-
Cite
Cite
Masoom Parwez, Tanweerul Huda, Kushal Mital, Bharati Pandya, Surgical technique: an improvisation in application of the technique of core-cut fistulectomy for fistula-in-ano, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab032, https://doi.org/10.1093/jscr/rjab032
Close - Share Icon Share
Abstract
Cryptoglandular fistula-in-ano is a chronic inflammatory condition of the perianal region attributed to the obstruction of the glands, located chiefly at the dentate line and their subsequent infection. Anal fistulae are difficult to treat, and minimally invasive procedures are evolving with promises. We present an improvised application of core-cut technique of fistulectomy. It is a minimally invasive, simple, effective and easy to perform procedure with minimal risk of incontinence and recurrence in simple cryptoglandular fistulae-in-ano. We performed 47 cases with good results and present this procedure to emphasize the procedural modification used.
INTRODUCTION
The global incidence of fistula in ano is 8.6 per 100 000 per year, of which 26–38% develop from previous perianal abscesses [1, 2]. Fistula-in-ano is a result of obstruction of the glands, located chiefly at the dentate line, by debris and their subsequent infection. It could also be due to previous surgeries, trauma, malignancy, diseases like Crohn’s, tuberculosis, HIV infections, etc. There are many surgical options available as not a single technique is fool proof. Conventionally successful techniques, like laying open of the tract (fistulotomy) and coring out the tract (fistulectomy) and cutting seton placement are fraught with complications ranging from recurrences to incontinence [3–5]. To overcome these complications, newer sphincter-saving procedures are fast evolving.
We present: The improvisation in the application of the technique of core-cut fistulectomy:
Indications: The Park’s classification describes fistula-in-ano as (i) superficial, (ii) intersphincteric, (iii) trans-sphincteric, (iv) suprasphincteric and (v) extrasphincteric [6, 7]. The complex fistulae (again 15–20%) need selective approaches. The superficial and low-lying inter- and trans-sphincteric fistulae are the most common (80–85%). Fistulotomy is best suited for the superficial variety which constitutes 15% of all fistulae [8]. The low-lying inter- and trans-sphincteric fistulae with straight tracts preferably up to 5–7 cm in length and 3–5 mm in diameter do exceptionally well with core-cut technique, even if the fistula is recurrent.
Instruments: Our instrument set (Fig. 1) was akin to the FiXcision device with slight modification in the diameter of the core-cutting circular blades [9]. It consisted of (1) probe with olive-tip on the proximal and screwable distal end, (2) the metallic guide-rod, (3) circular cutting blade with grip in three sizes, 5, 7 and 9 mm and (4) endplate, fenestrated for grip, and screwable.
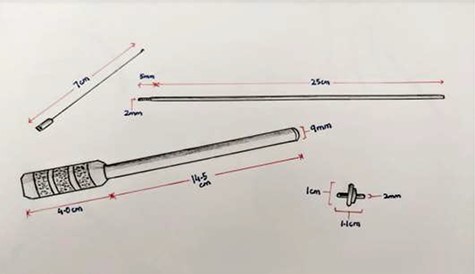
Instrument set consisted of (1) probe with olive-tip on the proximal and screwable distal end, (2) the metallic guide-rod, (3) circular cutting blade with grip in 3 sizes, 5, 7 and 9 mm and (4) endplate, fenestrated for grip, and screwable.
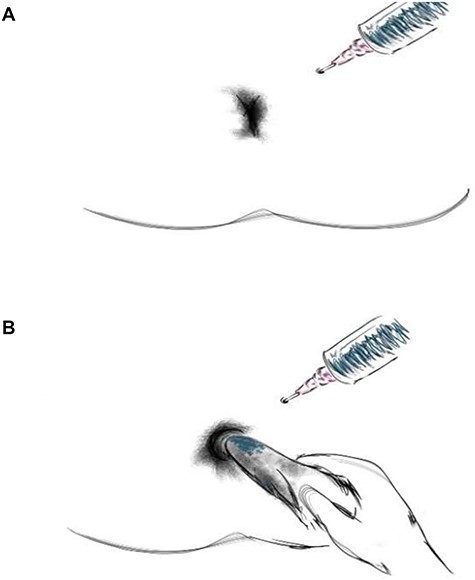
(A) Methylene blue is instilled via the external opening and (B) stain on the gauze piece checked.
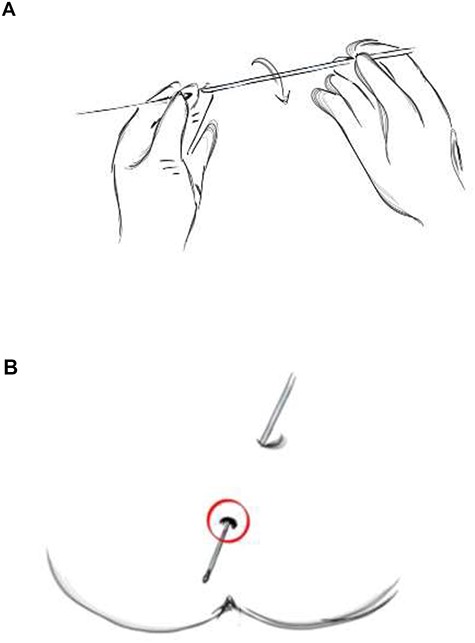
(A) The olive-tip probe is mounted on the guidewire, and (B) the tract probed till the olive-tip is seen at the internal opening.
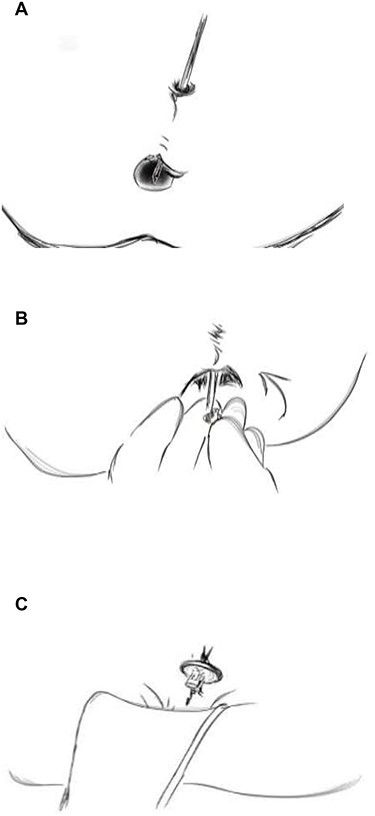
(A) Next, the olive-tip is dismantled and (B) replaced with the endplate by screwing it on to the guide-rod and the (C) rod gently pulled to snugly fit the endplate at the internal opening.

The circular cutter is next introduced over the rod and with rotatory movements propelled toward the endplate.

This action cores out the entire tract from external to internal opening. The rod when pushed forth displays the tract, the integrity of which is checked.
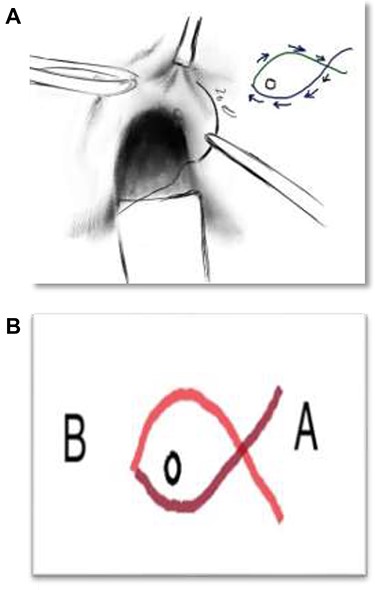
(A) ‘Fish-eye closure technique’. (B) To describe the details, (i) Vicryl 2/0 from point A to B, (ii) return from point B to A, (iii) 5 mm away from Internal opening, (iv) depth is up to internal sphincter muscle.
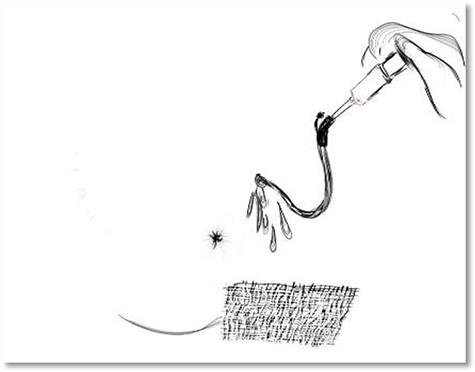
An infant feeding tube is used to flush the tract to remove clots and debris if any and this must be used for flushing daily to facilitate healing from inside-out.
Preoperative preparation: It is essentially an outpatient or day-care procedure. Work up is done with special emphasis on local examination to rule out abscesses and branching and to confirm either endoanal sonography or magnetic resonance imaging is performed [2]. The patients take a stimulant laxative the night before and are given an enema just prior to the surgery. Antibiotics are given 30 minutes before surgery.
Anesthesia: Pudendal block
The procedure:
Methylene blue is instilled via the external opening and stain on the gauze piece checked (Fig. 2A and B).
In cases where the internal opening is not obvious; persistent, gentle, push with added hydrogen peroxide is used to open the tract.
The olive-tip probe is mounted on the guidewire, to probe the tract till the internal opening (Fig. 3A and B).
Next, the olive-tip is dismantled and replaced with the endplate and the rod gently pulled to snugly fit the endplate at the internal opening (Fig. 4A–C).
The circular cutter is mounted and using rotatory movements propelled toward the endplate (Fig. 5).
Thus, the entire tract gets cored out. The tract integrity is checked (Fig. 6).
The most important step of closure of the internal opening is achieved by using our novel ‘Fish-eye closure technique’ (Fig. 7A and B).
The closure is tested by methylene blue reinstilled from External opening. To end the procedure an infant feeding tube is used to flush the tract to remove clots and debris and the tube needs daily flushing to facilitate healing from inside-out (Fig. 8).
Postoperative period: The patient stays for a few hours to maximum 24 hours. And on discharge is instructed to avoid constipation using osmotic laxatives at night. Twice daily Sitz baths are advised, and attendants trained to do the flushing of the tract with saline. Antibiotics are optional (Ciprofloxacin with metronidazole tablets), and analgesics are prescribed for 2–3 days.
Advantages of the procedure: It is a simple, office procedure, easy to learn, and reproducible. It is suitable for most of the simple fistulae (65–70%) [9]. No incontinence was noted. The recurrence rate is also low due to the technical simplicity of the procedure. The pain was mild to moderate and easily controlled with analgesics for a few days. The patient satisfaction as well as compliance was good.
DISCUSSION
Having studied the valuable experiences of our predecessors in treating fistula-in-ano, we realized that most fistulae were simple and could do well if the entire tract was removed, and the internal opening appropriately tackled. Thus, we decided to undertake a study to evaluate the basic necessity of modifications in the closure technique of the internal opening and also modified an instrument originally devised by AMI, FiXcision using circular cutting blade with different diameters tailored as per the particular fistula thickness, to avoid leaving behind parts of the tract, which we feel causes recurrence [10]. We also realized that fool-proof closure of the internal opening and flushing out the redundant cored out distal part of the tract was integral for healing. The intrinsic built of this instrument itself was suited to prevent incontinence. However, we played it safe by doing only simple cryptoglandular fistulae with short, straight tracts to begin with. We did 47 patients with this technique and only four patients had a recurrence on over a year-long follow-up, and none developed incontinence.
CONCLUSION
Anal fistula surgery poses several challenges. Minimally invasive procedures are taking over its treatment and we have presented a successful and satisfactory modification in the application of core-cut technique on 47 patients. We would further explore its applicability for more complex fistulae. Multicentric comparative studies and randomized trials are however needed to validate the efficacy of this procedure.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



