-
PDF
- Split View
-
Views
-
Cite
Cite
Xia Wu, Shun Li, Chang-Li Xie, Xiaoping Tang, Temporal lobe meningioma concurrent with multiple intracranial aneurysms, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa581, https://doi.org/10.1093/jscr/rjaa581
Close - Share Icon Share
Abstract
Aneurysms in the internal carotid artery, specifically the ophthalmic artery segment, have a lower incidence than any other type of aneurysm. Cases showing simultaneous intracranial aneurysms and meningiomas are extremely rare. This report shares a case of an adult female diagnosed with a deep temporal lobe meningioma concurrent with bilateral internal carotid artery-ophthalmic segment aneurysms. One-stage surgery with coronal incisions and a right frontotemporal craniotomy was performed for this patient. The lesion was first removed along the tumor margin, and the anterior clinoid process was removed. The aneurysm was clipped using an aneurysm clip. The frontal lobe was lifted from the right side, the optic chiasm was separated, the left internal carotid artery was exposed and ophthalmic segment of the left internal carotid artery aneurysm was clipped using a combination of two cross-vessel clips.
INTRODUCTION
There are only ~ 0.3–0.7% of meningioma cases that also exhibit multiple intracranial aneurysms. The pathogenesis of brain tumors associated with cerebral aneurysms is still unclear and is generally considered as incidental [1–3]. Here, we report a case of a patient who exhibited a temporal lobe meningioma showing multiple intracranial aneurysms. The right frontotemporal approach was used to successfully complete resection of the meningioma and clipping of the bilateral internal carotid artery-ophthalmic segment aneurysms. The patient showed no neurological defects after surgery.
CASE REPORT
A 52-year-old female patient was admitted to the neurosurgery department of our hospital for a recurring headache, dizziness, and the appearance of a black shadow in the right eye experienced over 1 month. The patient had a history of hypertension, long-term use of amlodipine benzenesulfonate tablets, and self-reported blood pressure control. She was unable to tolerate magnetic resonance imaging (MRI). An enhanced computed tomography (CT) scan of her head revealed a clear circular shadow in the right temporal region of the brain. The shadow contained a diameter of ~ 1.9 cm and lesions were apparent with no obvious signs of edema. CT angiography (CTA) revealed small saclike projections in the supraocular segment of the bilateral internal carotid artery with diameters of ~ 0.3 cm. A digital subtraction angiography (DSA) revealed a cystic shadow with a size of ~ 3.2 × 3.8 mm and a cervical width of ~ 2.4 mm visible in the ophthalmic segment of the right internal carotid artery protruding upward and outside the vascular lumen. The left ophthalmic artery, showing a size of ~ 3.0 × 4.2 mm and a cervical width of ~ 2.6 mm, was seen at the beginning of the lobulated cyst-like process from outside of the lumen. The ophthalmic artery rose from below the neck of the aneurysm (Fig. 1a–d).
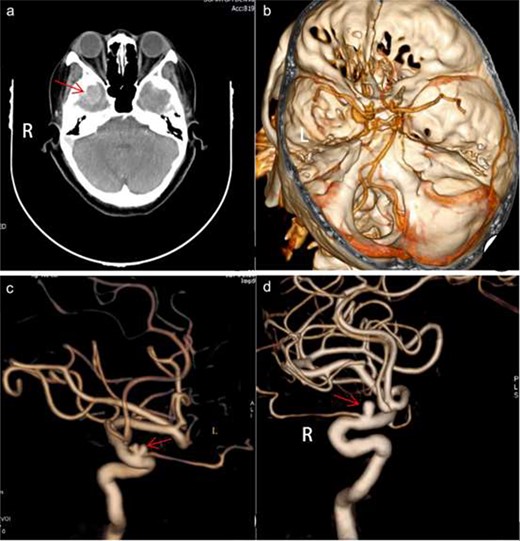
Preoperative imaging. axial CT demonstrated a clear circular shadow with a diameter of ~ 1.9 cm (a). A presurgical CTA revealed small cystic projections in the supra segment of the bilateral internal carotid artery bed process with a uniform diameter of 0.3 cm (b). Presurgical DSA revealed a cystic shadow that was visible in the ophthalmic segment of the right internal carotid artery protruding outside of the vascular lumen. The left ophthalmic artery was visible at the front of the lobulated cyst-like process arising from outside of the lumen. The ophthalmic artery rose from below the neck of the aneurysm (c and d). L, left; R, right.
Preoperative imaging examinations, general physical condition and family history of the patient were considered when deciding to perform one-stage operation by coronal incision using a right frontotemporal craniotomy. First, the right zygomatic arch was removed and a bone flap was formed. After hanging the dura, it was cut open to detect lesions, and the tumor was excised along the edge of the lesion. Subsequently, the lesion was repeatedly cauterized at the base of the dura mater using noncondensable bipolar electrocoagulation tweezers. Furthermore, the lateral fissure was separated to expose the internal carotid artery. The aneurysm in the ophthalmic segment of the right internal carotid artery was blocked by the clinoid process, which was removed to expose the proximal and distal ends of the aneurysm. The aneurysm was clipped using an aneurysm clip. The frontal lobe from the right side was raised, the optic chiasm was separated, the left internal carotid artery was exposed, the ophthalmic segment left internal carotid artery aneurysm was detected and the aneurysm was clipped using a combination of two cross-vessel clips (Fig. 2a–f). Figure 3a and b shows a representation of the postoperative pathological diagnosis of the fiber type meningioma (WHO I Level). A postoperative CTA showed complete occlusion of the ophthalmic segment aneurysm of the bilateral internal carotid artery and a CT scan revealed postoperative changes in the right temporal bone, swelling of adjacent scalp soft tissues, and slight gas accumulation (Fig. 4a and b). The patient recovered well from the procedure and was discharged from the hospital.
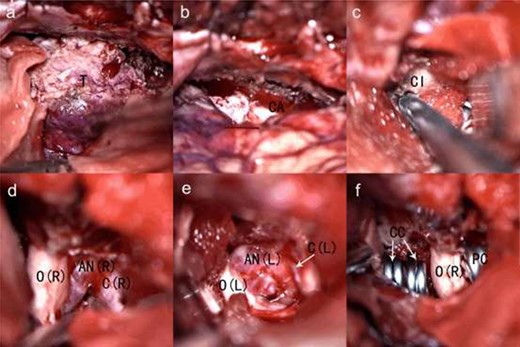
The intraoperative view (a–f). T, tumor; CA, tumor cavity after resection; Cl, clinoid; O(R), right optic nerve; AN (R), right internal carotid artery-ophthalmic segment aneurysms; C(R), right internal carotid artery; O(L), left optic nerve; AN(L), left internal carotid artery-ophthalmic segment aneurysms; C(L), left internal carotid artery; CC, combination of 2 cross—vessel clips; PC, permanent clip.
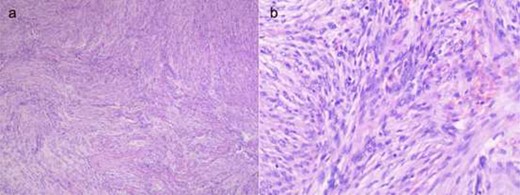
Representative fibroid meningioma shown by hematoxylin and eosin staining. (a) ×40 magnification and (b) ×200 magnification.
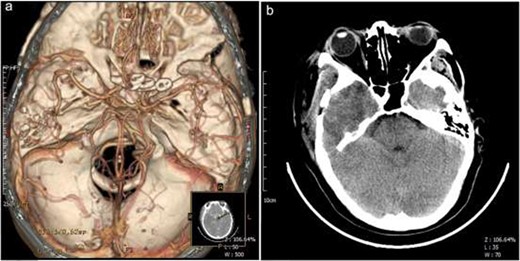
Postoperative imaging. Postsurgical CTA revealed that bilateral ophthalmic segment internal carotid artery aneurysms were completely obliterated (a); Postsurgical CT showed postoperative changes in the right temporal bone, swelling of adjacent scalp soft tissues, and slight gas accumulation (b). A, anterior; P, posterior; L, left; R, right.
DISCUSSION
Intracranial meningiomas simultaneously present with intracranial aneurysms are not commonly observed in the clinic. In the case presented here, meningioma symptoms appeared earlier than symptoms of aneurysms. Therefore, the diagnosis of patients with tumors associated with unruptured aneurysms needs to be improved using brain CT, MRI, CTA or DSA procedures [4, 5]. Symptomatic intracranial aneurysms and meningiomas, especially ruptured aneurysms, need to be treated quickly. When the asymptomatic intracranial aneurysm exhibits an irregular shape, there is a greater risk of rupture, indicating the need for active treatment [6, 7]. Asymptomatic aneurysms that are small in size and show regular morphology should be treated based on location, risk factors, patient age, the general condition of the patient and surgical difficulty [8]. If two lesions are adjacent to one other or if one surgical approach can be achieved at the same time, corresponding treatment should be performed. If a surgical approach cannot be completed, stage surgery treatment should be used. The treatment choice of paraclinoid aneurysms is controversial. Although endovascular treatment is easier to reach the aneurysm site, the rate of complete aneurysm neck occlusion is low, and recurrence is high, and mass effect cannot be clearly reduced. The cure rate of craniotomy clipping is relatively high and recurrence rate is low, the mass effect can be obviously relieved and ocular symptoms can be improved, but it is difficult to establish proximal control, and the risk of separation and anatomical exposure is high. Intraoperative balloon occlusion of the near segment of the internal carotid artery should be used. In the case presented here, the patient developed a headache, dizziness and the appearance of dark shadows observed out of the right eye. Both CTA and DSA examinations revealed the presence of an irregular and lovulated aneurysm that contained a thin cyst wall. The patient was unable to afford surgical expenses. After comprehensive consideration, one-stage surgery was performed on the patient using a coronary incision and right frontotemporal approach for tumor resection and then to clip the bilateral internal carotid artery-ophthalmic segment aneurysms. Complicated anatomy and other factors make it difficult to directly clip aneurysms. Here, we simultaneously clipped the ophthalmic segments of the internal carotid artery aneurysms on both sides. This operation was extremely challenging but was successful because the meningioma was completely removed and the patient showed no neurological defects after the procedure.
CONCLUSION
Meningioma cases showing multiple intracranial aneurysms have a very low incidence and exhibit an unknown pathogenesis. Brain CT, MRI, CTA or DSA procedures should be improved to avoid adverse consequences related to diagnosis and treatment. Surgical treatment should be based on a variety of measures, including the size of the meningioma and intracranial aneurysms, their locations, the difficulty of clipping aneurysms, the general condition of the patient and the economic background as well as financial status of the patient.
AUTHORS’ CONTRIBUTIONS
X.W. did the manuscript writing. C.-L.X. collected case data. S.L. did the manuscript review. X.T. did the conception of idea and supervision of the project. All authors read and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
All the authors declare no conflict of interest.
FUNDING
No funding was obtained for this study.
AVAILABILITY OF DATA AND MATERIALS
The data was obtained from the patient’s surgical records and the picture obtained with the consent of the patient.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the participant included in the study.



