-
PDF
- Split View
-
Views
-
Cite
Cite
Arin Mahmoud, Arun Kozhikunnath, Pranai Buddhdev, The successful use of collagenase for Ledderhose disease (plantar fibromatosis) in a paediatric patient: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa501, https://doi.org/10.1093/jscr/rjaa501
Close - Share Icon Share
Abstract
Ledderhose disease is a connective tissue disorder involving proliferation of fibrous tissue in the plantar fascia of the foot. Histologically identical manifestations exist in the hand (Dupuytren’s contracture) and penis (Peyronie’s disease), and collagenase injections are approved as a treatment in both, however not in Ledderhose, where the treatment of choice remains surgical resection. Surgery is associated with high rates of recurrence and need for further surgery, so alternative therapies should be sought. Due to their histological and physiological similarities, it is likely that therapies useful in Dupuytren’s and Peyronie’s would be useful in Ledderhose. Two previous case reports investigating collagenase injections for Ledderhose disease in adults have shown conflicting results; this study demonstrates the efficacy of collagenase injections in a paediatric patient at 1-year follow-up.
INTRODUCTION
Ledderhose disease (LD), or plantar fibromatosis, is a benign disease characterized by hyperproliferation of the fibrous tissue of the plantar fascia. The disease is a singular manifestation of a systemic connective tissue disorder including Dupuytrens contracture (DC) and Peyronies disease (PD), which affect the palmar fascia and tunica albugenia, respectively. These clinical manifestations are often bilateral and concomitant [1]. The cause of these diseases remains unknown [1, 2].
The tissue changes in this family of diseases are histologically identical [1], with excessive proliferation of fibroblasts and myofibroblasts and dense bands of collagen in mature lesions [3]. LD tends to present with nodules affecting the medial and central aspect of the plantar aponeurosis, without typically progressing to a cord or cause a contracture as in DC. These nodules can cause symptomatic discomfort and impede weight bearing activities.
LD is less prevalent than DC, with a ratio of 1:5–1:10 [1]. The aetiology is deemed similar; both affecting predominantly Northern European, middle-aged males. They are commonly associated with each other in addition to frozen shoulder, diabetes mellitus, epilepsy, repetitive/overuse trauma and excess of alcohol and nicotine [1, 2].
Treatment strategies for LD include conservative, medical and surgical. As the disease carries no morbidity, if symptoms are mild, management may be limited to conservative measures such as orthopaedic insoles and physical therapy [2]. Medical treatments suggested as beneficial for LD include topical or injected steroids [2], which are used in DC, but little evidence exists for their efficacy in LD. Surgical management is the mainstay of treatment, but is associated with high rates of recurrence, ranging from 60 to 84% [4–6].
With the unacceptably high recurrence rates associated with surgical excision, in addition to other standard surgical risks, there is room for the development of effective medical therapies. Collagenase (Clostridium histolyticum) injections have been shown to be effective in treating DC and PD [7], and is licenced in the UK and USA. In next section we present the first case report evaluating the efficacy of collagenase Clostridium histolyticum (CCH) in the treatment of LD in a child.
CASE REPORT
A Caucasian 13-year-old female was referred to our orthopaedic service for assessment of a painful lump on the sole of the left foot, causing pain on ambulation. Clinical examination demonstrated a 20 × 10 mm nodule on the plantar aspect of the foot with tenderness on deep palpation. Ultrasonographic evaluation confirmed the presence of a fibroma attached to the plantar fascia measuring 14 × 4 × 9 mm (Fig. 1).
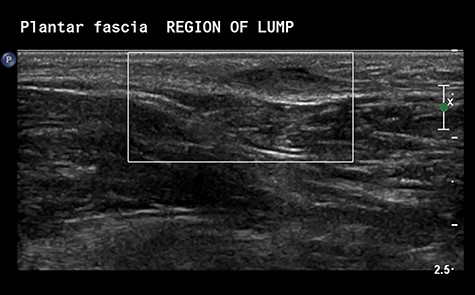
Ultrasonographic Images demonstrating the presence of a nodule embedded in the plantar fascia.
With a radiological diagnosis of LD, the management options were discussed with the patient and her family, who agreed to proceed with surgical excision. A wide local excision was performed; the tissue sent for histopathological analysis, which confirmed the diagnosis of LD (Figs 2 and 3).
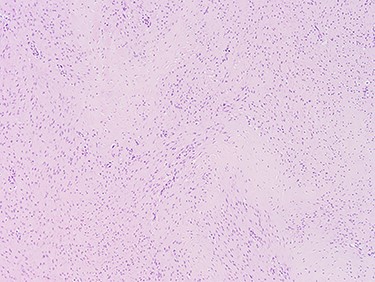
Images at ×4 magnification. Tissue samples comprise of cytologically bland spindle cell proliferative features which extends into the adjacent fibrofatty tissue.
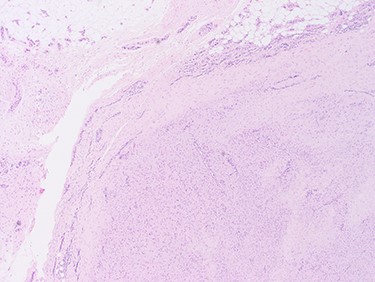
The cellular pattern is haphazard with areas of dense fibrosis, suggestive of fibromatosis (LD).
One-year post-surgery, the patient returned to the orthopaedic clinic with a local recurrence of a tender 40 × 20 mm nodule and worsening symptoms. The Foot and Ankle Outcome Score (FAOS) was 238/500. The lead physician discussed her case at a specialist regional Multi-discipliniary Meeting (MDT) and with the family, obtaining consent for an attempt of a single off-label use of CCH. Permission was granted through the Trust formulary pathway.
The intralesional CCH injection was performed under general anaesthetic; multiple injection sites were used to ensure sufficient concentration of delivery. Post-operative weight-bearing was permitted, and daily stretching encouraged. At 3 weeks review, significant improvement was noted with a reduction in size of the nodule and no tenderness on palpation. Further review at 4 months and then at 1 year demonstrated sustained resolution of symptoms, return to activity and a FAOS of 448.5/500.
DISCUSSION
This case report demonstrates the efficacy of CCH injections for LD in a paediatric patient.
Surgical management including wide local excision and subtotal/total plantar fasciectomy has been the mainstay of treatment of LD worldwide [5]. One study involving 33 feet in 27 patients reported an overall recurrence rate of 60%, highest for local excision (100%) and lowest in total fasciectomies (25%) [6]. The trend of local excision being associated with higher recurrence rates is borne out in other literature [5]. One study reduced recurrence rates with adjunct radiotherapy, albeit with worse functional outcomes [8]. Another study demonstrated high rates of recurrence (32/38) following primary excision in children aged 2–12, with follow-up ranging from 4 months to 33 years; 19 patients required repeat surgery within 12 months [4].
Despite National Institute of Clinical Excellence (NICE) approval for its use in two pathologically similar conditions, there is little evidence regarding the use of CCH in LD. Currently two cases describing CCH injections for LD exist in the literature, both for adults. The first was a 72-year-old male with bilateral DC, left sided LD and recurrence following steroid injections and a partial plantar fasciectomy [9]. Despite three collagenase injections at 1-month intervals, no significant improvement was noted; the authors acknowledge not performing passive extension of the fibrous plaque due to the absence of a palpable cord, as in DC, and speculate anatomical differences in the plantar region account for the lack of success.
The second case report was in a 20-year-old female, who underwent three surgical procedures for LD following unsuccessful physical therapy and steroid injections [10]. With recurrence of symptomatic nodules, CCH injection was performed with toe extension exercises and plantar massage the next day. At the 30-day follow-up, sustained to 7 years, the patient reported to be symptom free with no recurrence. This highlights the importance of post-operative stretching and massage.
This case report demonstrates successful treatment of LD with a single, minimally invasive injection of CCH, in a patient who had proven resistance to surgical treatment. Following on from its approval for use in DC and PD, CCH has the potential to be of comparable benefit in LD.



