-
PDF
- Split View
-
Views
-
Cite
Cite
Wendy Chang, Mieko Udo, Bettina Schulze, A case of spontaneous idiopathic tension pneumoperitoneum successfully managed with bedside pig-tail catheter, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab528, https://doi.org/10.1093/jscr/rjab528
Close - Share Icon Share
Abstract
We present a 67-year-old gentleman with a high perioperative mortality and morbidity risk who presented with spontaneous idiopathic tension pneumoperitoneum that was successfully managed with bedside pig-tail catheter insertion. Here we also discuss other potential non-surgical aetiologies of pneumoperitoneum.
INTRODUCTION
Pneumoperitoneum or air within the abdominal cavity is not always a result of perforated viscous. However, it does account for 85–95% of pneumoperitoneum cases, and early involvement of surgeon for potential laparotomy is of paramount importance. The remaining non-surgical aetiologies of pneumoperitoneum are divided into different categories: thoracic, abdominal, gynaecological and very rarely idiopathic. Spontaneous idiopathic pneumoperitoneum is rare [1–4], and idiopathic tension pneumoperitoneum is an even rarer entity.
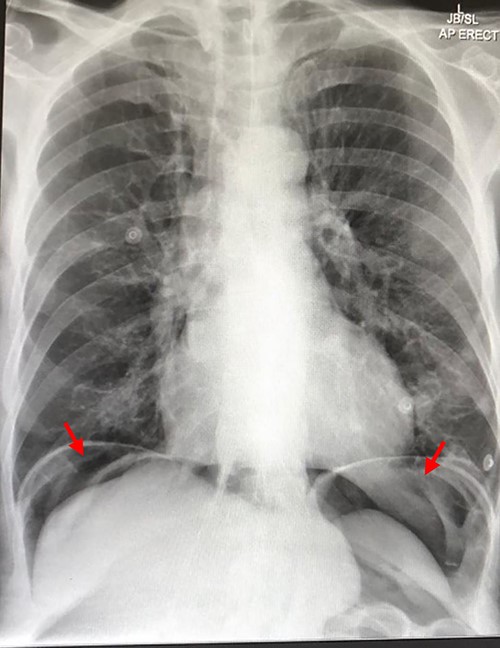
Chest X-ray showing air under the diaphragm suggestive of pneumoperitoneum (red arrows)

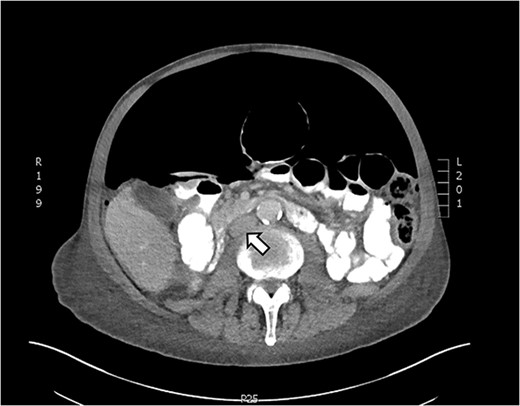
CT scan on initial presentation showing pneumoperitoneum without obvious cause. Sagittal, axial, coronal views. Arrows show pockets of free intraperitoneal air
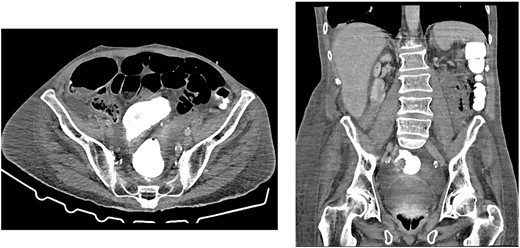
Axial CT showing tension pneumoperitoneum and collapsed inferior vena cava (arrow)
CASE
A 67-year-old man presented to the emergency department with shortness of breath with increased work of breathing and right-sided shoulder pain radiating to the right lower quadrant of the abdomen for three days. His history included 50 pack-year smoking history resulting in severe COPD with FEV1 of 18%, and newly diagnosed base of tongue squamous cell carcinoma with metastasis to his lungs. He was on palliative chemotherapy. In addition, he had a rectosigmoid adenocarcinoma 3 years ago, managed with laparoscopic-assisted anterior resection. He had follow-up colonoscopies and flexible sigmoidoscopy confirming healthy mucosa and patent anastomosis. His most recent flexible sigmoidoscopy, confirming healthy anastomosis was 5 days prior to presentation.
| Thoracic |
| • Bronchopulmonary fistula |
| • Rupture of pulmonary blebs |
| • Barotrauma: |
| • Scuba diving (Schriger et al.) |
| • Mechanical ventilation |
| • Positive pressure ventilation |
| • Cardiopulmonary resuscitation |
| • Pneumothorax |
| • Pneumomediastinum |
| Abdominal |
| • Pneumatosis cystoides |
| • Peritoneal dialysis |
| • Recent open abdominal surgery |
| • Endoscopic procedures |
| • Postpolypectomy syndrome |
| • Recent open laparotomy |
| • Recent laparoscopy |
| Gynaecological |
| • Vaginal douching |
| • Gynaecological procedures |
| • Intercourse |
| • Pelvic inflammatory disease |
| Idiopathic |
| Thoracic |
| • Bronchopulmonary fistula |
| • Rupture of pulmonary blebs |
| • Barotrauma: |
| • Scuba diving (Schriger et al.) |
| • Mechanical ventilation |
| • Positive pressure ventilation |
| • Cardiopulmonary resuscitation |
| • Pneumothorax |
| • Pneumomediastinum |
| Abdominal |
| • Pneumatosis cystoides |
| • Peritoneal dialysis |
| • Recent open abdominal surgery |
| • Endoscopic procedures |
| • Postpolypectomy syndrome |
| • Recent open laparotomy |
| • Recent laparoscopy |
| Gynaecological |
| • Vaginal douching |
| • Gynaecological procedures |
| • Intercourse |
| • Pelvic inflammatory disease |
| Idiopathic |
| Thoracic |
| • Bronchopulmonary fistula |
| • Rupture of pulmonary blebs |
| • Barotrauma: |
| • Scuba diving (Schriger et al.) |
| • Mechanical ventilation |
| • Positive pressure ventilation |
| • Cardiopulmonary resuscitation |
| • Pneumothorax |
| • Pneumomediastinum |
| Abdominal |
| • Pneumatosis cystoides |
| • Peritoneal dialysis |
| • Recent open abdominal surgery |
| • Endoscopic procedures |
| • Postpolypectomy syndrome |
| • Recent open laparotomy |
| • Recent laparoscopy |
| Gynaecological |
| • Vaginal douching |
| • Gynaecological procedures |
| • Intercourse |
| • Pelvic inflammatory disease |
| Idiopathic |
| Thoracic |
| • Bronchopulmonary fistula |
| • Rupture of pulmonary blebs |
| • Barotrauma: |
| • Scuba diving (Schriger et al.) |
| • Mechanical ventilation |
| • Positive pressure ventilation |
| • Cardiopulmonary resuscitation |
| • Pneumothorax |
| • Pneumomediastinum |
| Abdominal |
| • Pneumatosis cystoides |
| • Peritoneal dialysis |
| • Recent open abdominal surgery |
| • Endoscopic procedures |
| • Postpolypectomy syndrome |
| • Recent open laparotomy |
| • Recent laparoscopy |
| Gynaecological |
| • Vaginal douching |
| • Gynaecological procedures |
| • Intercourse |
| • Pelvic inflammatory disease |
| Idiopathic |
On presentation, his temperature was 37.8°C, and he was hypotensive at 100/45 mmHg and tachypneic with a respiratory rate of 22. He was in moderate respiratory distress and was placed on 2 L oxygen via nasal prongs. On abdominal examination, mild distension was noted with lower abdominal tenderness with rebound tenderness and guarding in the right lower quadrant. He had normal leukocytes of 5 × 109 /L (N: 4.0–11 × 109/L) and lactate was normal at 1.6 mmol/L (N: 0.5–2.2 mmol/L). X-ray chest showed free air under the diaphragm suggestive of pneumoperitoneum (Fig. 1). A CT abdomen was performed showing large-volume free air suggestive of a viscous perforation and moderate volume of free fluid in the abdomen (Fig. 2). The site of perforation was not confidently established on the study. There was generalized oedema of the right side of the colon with multiple loops of dilated small bowel. His Physiological and Operative Severity Score for enumeration of Mortality and Morbidity (POSSUM) score would be 81% predicted mortality and 98.8% predicted morbidity if he were to undergo an emergent laparotomy operation. Family discussion was made, and he decided not to proceed with operative management. He was managed conservatively with piperacillin-tazobactam and decompressed with nasogastric tube insertion. As the days progressed, his abdomen became increasingly distended and tympanic, but not peritonitic. We repeated a CT chest and abdomen three days after initial admission and it was reported he had tension pneumoperitoneum (Fig. 3). CT with oral contrast was also performed to exclude an upper GI perforation.
His abdomen was emergently decompressed over the evening; however, within 12 h, the pneumoperitoneum had recurred. We then inserted a 14.0 Fr, 29 cm pig-tail catheter at bedside (Fig. 4). It was then connected to an intercostal catheter (ICC) drain. Immediately, a gush of air was released, there was bubbling in his chest drain and his abdomen immediately became less tense. As no obvious site of viscous perforation was identified on imaging, we decided to explore other causes of pneumoperitoneum. These included severe COPD, broncho-peritoneal fistula, bullous emphysema and anastomotic leak [5–7]. Cardiothoracic surgeons (CTS) were consulted regarding potential thoracic causes of his pneumoperitoneum given his background of severe emphysema but was deemed highly unlikely by both the CTS and radiologists as his CT chest did not show a large bullae or broncho-peritoneal fistula and he was not mechanically ventilated. A CT with rectal contrast was performed to exclude anastomotic leak from the rectal anastomosis, and there was no evidence of contrast extravasation into the peritoneum at the anastomosis site (Fig. 5). The pig-tail catheter was in place for 3 days and then clamped for two days without any re-accumulation of the pneumoperitoneum, the pigtail was removed and the patient was discharged without further complications.

CT showing resolution of the tension pneumoperitoneum post pig-tail insertion and anastomotic integrity—no leakage of contrast
DISCUSSION
Pneumoperitoneum commonly occurs following perforated viscous or a history of recent operation resulting in accumulation of residual air. It is often considered to be a surgical emergency with a need for an urgent exploratory laparotomy. However, there are also many non-surgical aetiologies of pneumoperitoneum. Patients with non-surgical causes of pneumoperitoneum are generally patients who do not present with signs of perforated viscous such as peritonitis, leukocytosis or fever. As a result, this can often present as a diagnostic and management dilemma for medical physicians and surgeons [8]. Non-surgical causes of spontaneous pneumoperitoneum are grouped into several categories: intrathoracic, intra-abdominal, barotrauma [9], gynaecological, pneumatosis cystoides, and idiopathic (Table 1). For our patient, his pneumoperitoneum may have been a result of the flexible sigmoidoscopy he had 5 days prior to presentation; however, there have been no documented cases during our literature search.
Here, we present a case of spontaneous idiopathic pneumoperitoneum with CT findings of tension pneumoperitoneum managed successfully with bedside decompression using a pig-tail catheter attached to a chest drain. Failure of decompressing the tension pneumoperitoneum may result in hemodynamic instability and ischemia of abdominal organs as large pneumoperitoneum may compress on the inferior vena cava reducing venous return to the heart. CT findings of tension pneumoperitoneum include marked elevation of diaphragm, decreased thoracic volume and/or compression of the inferior vena cava [10]. Emergency percutaneous needle compression using 16G cannulas have been used in cases for immediate decompression of the tension pneumoperitoneum [11]. Our patient had a high POSSUM score; for him to undergo a laparotomy would place him at a high mortality and morbidity risk. Here we demonstrate successful management of idiopathic tension pneumoperitoneum with pig-tail catheter attached to an intercostal drain.



