-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihiro Tatekawa, Surgical approach to three pediatric patients with ovarian tumors: laparoscopic excision using a specimen retrieval bag, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab505, https://doi.org/10.1093/jscr/rjab505
Close - Share Icon Share
Abstract
We report our experience with three pediatric patients with ovarian tumors who underwent laparoscopic excision using a specimen retrieval bag. Patient 1 was a 12-year-old girl with a left ovarian tumor. The tumor was laparoscopically placed in a specimen retrieval bag and removed through a suprapubic incision without content spillage. Patient 2 was a 14-year-old girl with a left ovarian tumor. The tumor was laparoscopically placed in a specimen retrieval bag. The contents of the tumor were aspirated, and the tumor was removed without content spillage. Patient 3 was a 13-year-old girl with bilateral large ovarian tumors. After releasing torsion of the left-sided mass, each tumor was laparoscopically placed in a specimen retrieval bag and excised. Peritoneal lavage was performed due to content spillage. The pathologic findings confirmed mature teratomas in all patients. All three girls have been doing well without evidence of chemical peritonitis or recurrence.
INTRODUCTION
Ovarian mature cystic teratomas (MCTs), also called dermoid cysts, represent 70% of all benign ovarian masses that occur during the reproductive years. They are responsible for 50% of pediatric tumors [1–8].
The laparoscopic approach is generally considered the standard of care for benign ovarian masses [1–5]. Oophorectomy is the definitive treatment, but ovarian cystectomy is recommended in younger women and girls. Although laparoscopic surgery has many benefits, it carries the risk for chemical peritonitis with content spillage. Various techniques have been used to reduce this risk, including routine intraoperative use of an endoscopic retrieval bag [1–5].
CASE SERIES
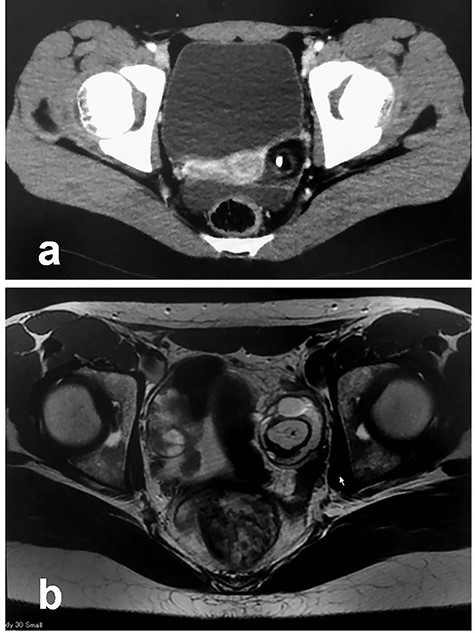
Patient 1: In a 12-year-old girl with abdominal pain, enhanced computed tomography (CT) showed a swollen appendix and a left ovarian mass; she was diagnosed with appendicitis (Fig. 1a). After laparoscopic appendectomy, she underwent magnetic resonance imaging (MRI), which revealed an ovarian MCT (38 cm × 30 cm; Fig. 1b). She underwent a second procedure, laparoscopy-assisted extracorporeal cystectomy (a hybrid, minimally invasive approach), during which the tumor was placed in a specimen retrieval bag and exteriorized through a suprapubic incision. The tumor was then excised, and the ovary returned to the pelvis. There was no content spillage (Fig. 2). The excised margins of the tumor were continuously oversewn using absorbable suture. Pathologic examination confirmed the diagnosis of MCT. The patient has been doing well without evidence of recurrence. She subsequently established a regular menstrual cycle.
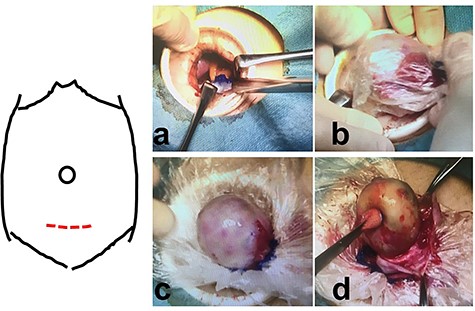
Intraoperative findings in Patient 1; (a–c): A suprapubic incision, with wound retractor, is used for removal of the specimen that was previously placed in a specimen retrieval bag; (d): Ovarian cystectomy is performed inside the specimen retrieval bag without content spillage.
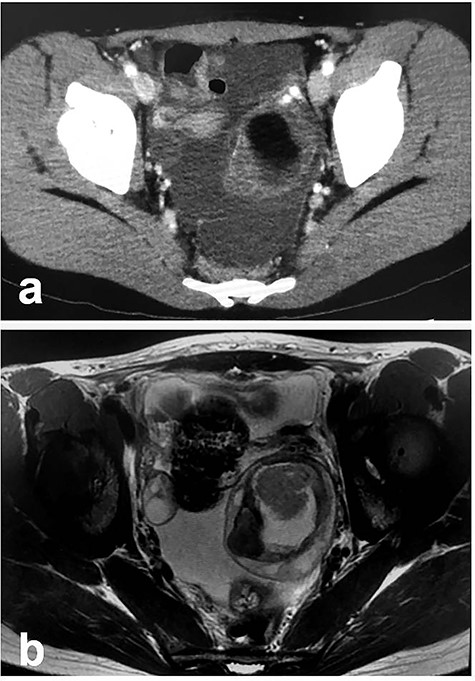
Patient 2: In a 14-year-old girl with abdominal pain, enhanced CT showed a left ovarian tumor (Fig. 3a). Further examination, including MRI, revealed an ovarian MCT (70 cm × 67 cm; Fig. 3b). She underwent laparoscopic surgery, during which the tumor was placed in a specimen retrieval bag. The contents were aspirated using a newly developed soft-cup aspirator set (Hakko Co., Tokyo, Japan) [9], and the tumor was excised without content spillage (Fig. 4). The excised margins were continuously oversewn using the V-Loc™ absorbable wound closure device (Covidien Healthcare, Minneapolis, MN). Pathologic examination confirmed the diagnosis of MCT. She has been doing well without evidence of recurrence. She subsequently established a regular menstrual cycle.
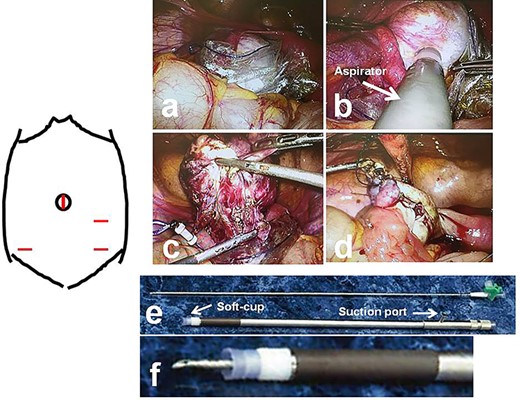
Intraoperative findings in Patient 2; (a): The tumor is laparoscopically placed in a specimen retrieval bag; (b): A soft-cup aspirator set is attached to the surface of a tumor, and the contents are aspirated; (c): Ovarian cystectomy is performed laparoscopically, within the specimen retrieval bag, without content spillage; (d): The excised margins are continuously oversewn using an absorbable wound closure device; (e): The soft-cup aspirator set (upper, suction needle; lower, soft-cup aspirator); (f): Before attaching the soft-cup aspirator to a tumor, the suction needle is placed within the soft-cup aspirator, with the tip of the needle protected.
Patient 3: In a 13-year-old girl with abdominal pain, plain CT revealed bilateral ovarian tumors (Fig. 5a: left tumor and Fig. 5b: right tumor). Further examination, including MRI, revealed bilateral ovarian MCTs (Fig. 5c: left tumor; 77 cm × 70 cm, Fig. 5d: right tumor; 115 cm × 90 cm). During laparoscopic surgery, torsion of the left ovarian tumor was released, and each mass was placed in a specimen retrieval bag and removed (left tumor, Fig. 6a–d; right tumor, Fig. 6e–h). Both tumors were large, and content spillage was recognized during surgery. Peritoneal lavage was performed using large amounts of warmed fluid. Pathologic examination of both tumors confirmed the diagnosis of bilateral MCTs. The patient has been doing well without evidence of recurrence. She subsequently established a regular menstrual cycle.
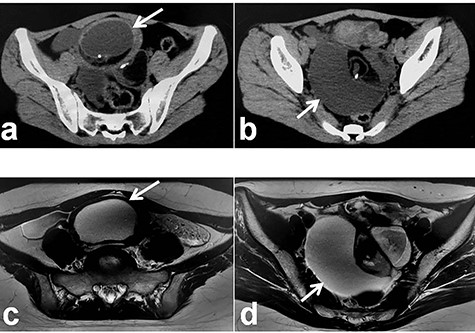
Radiologic findings in Patient 3; (a): Plain CT showing the left-sided tumor (white arrow); (b): Plain CT showing the right-sided tumor (white arrow); (c): MRI showing the left-sided tumor (white arrow); (d): MRI showing the right-sided tumor (white arrow).
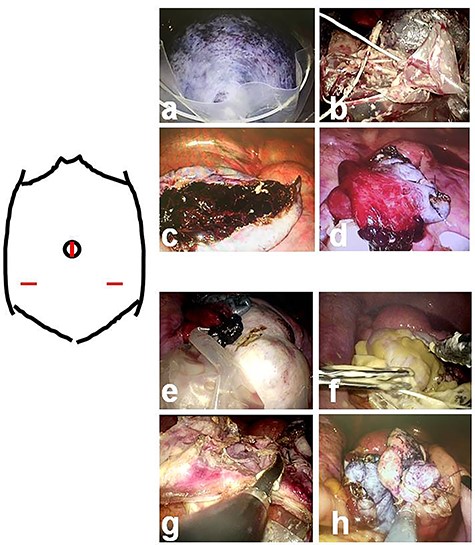
Intraoperative findings in Patient 3; (a–d): Left-sided tumor (e–h): Right-sided tumor After laparoscopically releasing torsion of the left ovarian tumor, each tumor is placed into a specimen retrieval bag and excised. When content spillage is recognized, peritoneal lavage is performed using large amounts of warmed fluid. The excised margins are continuously sutured using an absorbable wound closure device.
FOLLOW-UP
After surgery, our routine follow-up procedure is to use ultrasonography (US) every 6 months and MRI every 12 months. Serum tumor markers, such as squamous cell carcinoma (SCC) antigen, carcinoembryonic antigen (CEA), cancer antigen (CA) 19–9, CA 125, alpha fetoprotein (AFP) and the beta subunit of human chorionic gonadotropin (β-hCG) are examined every 6 months.
DISCUSSION
In the surgical approach to ovarian MCT, there is lack of consensus on whether laparoscopy or laparotomy is preferable. The maximum cyst size above which laparotomy should be considered is controversial. Some investigators recommended laparotomy for MCTs > 10 cm in diameter [1], but spillage is more likely in cysts with a diameter of 8 cm or greater. Oncologically, laparoscopy is considered safer for lesions of 8 cm or less [2]. In our three case reports, two of MCTs with a diameter of 8 cm or lesser could be resected successfully without spillage using a specimen retrieval bag, but another of MCT with a diameter of 8 cm or greater was resected with content spillage even if a specimen retrieval bag was used. Intraoperative findings showed tumor contents were filled with much yellowish, pasty sebaceous material and content spillage was recognized during laparoscopic surgery. If malignancy is considered likely in an ovarian tumor, laparotomy is appropriate for removal and staging; this minimizes the risk of intraperitoneal spillage of tumor contents. For tumors where the risk of malignancy is likely low but uncertain, a hybrid minimally invasive approach, such as laparoscopy-assisted extracorporeal cystectomy, may decrease the risk for intraperitoneal spillage of cyst contents [4]. In hybrid minimally invasive approach, the risk of intraoperative rupture was increased by laparoscopic approach compared with laparotomy. The risk of rupture of a benign tumor is low; however, the risk of rupture of a malignant would result in an upstaging. For this reason, if a tumor is likely to be malignant, laparotomy is appropriate for removal of the ovary and staging to minimize risk of intraperitoneal spillage of tumor contents. For tumors where the risk of malignancy is likely to be low but uncertain, many have advocated a hybrid minimally invasive approach, which may decrease the risk of intraperitoneal spillage of cyst contents [4].
Looking back, as a reflection point, In Patient 3 of our case reports, hybrid minimally invasive approach should be performed to decrease the risk for intraperitoneal spillage of cyst contents. Fortunately, usage of a specimen retrieval bag could minimize intraperitoneal spillage of cyst contents and peritoneal lavage was performed using large amounts of warmed fluid with laparoscopic surgery.
Several studies comparing laparoscopy with laparotomy for ovarian MCT describe the benefits of laparoscopy as reduction of febrile morbidity and of postoperative pain and complications, overall cost, and earlier discharge from hospital [10]. Febrile morbidity was defined as at least one episode of temperature rise above 38°C in the 24 h. However, the laparoscopic approach carries a higher risk for content spillage and subsequent chemical peritonitis, and of recurrence when ovarian cystectomy is performed [1–5].
Various techniques are used to reduce the rates of spillage during laparoscopy, chemical peritonitis and recurrence after laparoscopy. One of these techniques, recommended by many researchers, is the routine intraoperative use of an endoscopic retrieval bag [1–5]. In this method, the cyst is placed into the bag before it is punctured and aspirated. Any material that happens to leak out of the bag is easier to suction than spillage that occurs during laparotomy [1]. The risk for chemical peritonitis after content spillage can be overcome with thorough peritoneal lavage using warmed fluid [1–5]. Use of an irrigation cannula with jet-wash lavage is an effective cleaning method that may not be available during laparotomy [5].
Patients with MCT are reportedly at risk for a contralateral teratoma at a median of 3 years after initial oophorectomy. Although the risk for ipsilateral recurrence is low after cystectomy, postoperative US monitoring of both ovaries is recommended. Ovarian-sparing surgery is preferable for patients with MCTs, given the risk for a contralateral de novo neoplasm [4].
Most MCTs occur in younger patients, in whom malignant transformation is rare; when it does occur, the most common manifestation is SCC [6–8]. Malignant transformation reportedly occurs in 0.17–2% of MCTs and mainly happens in women older than 50 years of age [6–8]. The role of tumor markers has not been fully established in the assessment and follow-up of MCTs. Higher levels of CA 125 have been associated with adverse outcomes, but elevated CEA levels are reportedly more useful than either CA 125 or CA 19–9 in the diagnosis of malignant transformation of MCT [6]. On the other hand, levels of CEA, SCC antigen, CA125 and CA 19–9 are statistically significantly higher in patients with SCC arising from MCT than in those with uncomplicated MCT [7, 8]. Furthermore, levels of SCC antigen are elevated on serial monitoring in patients with SCC arising from MCT and in those whose tumors have recurred [8].
All three of our patients have been followed for >3 years after surgery, and all are doing well without evidence of recurrence. Their tumor markers have not increased and remain within normal limits.
DISCLOSURES
The author has no competing financial interests. The author alone is responsible for the content and writing of this manuscript.
CONFLICT OF INTEREST STATEMENT
The author has no conflicts of interest to declare.
FUNDING
The author received no funding in connection with this manuscript.



