-
PDF
- Split View
-
Views
-
Cite
Cite
Mirwais Khan Hotak, Mike He, Mixed serous and mucinous retroperitoneal cystadenoma: an extremely rare case, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab468, https://doi.org/10.1093/jscr/rjab468
Close - Share Icon Share
Abstract
Mixed serous and mucinous retroperitoneal cyst adenoma is an extremely rare condition as most of the reported cases in the literature are primary retroperitoneal mucinous cystadenomas and primary retroperitoneal serous cystadenomas. They are initially asymptomatic and become symptomatic gradually depending on their size and anatomical extension and location. We report a 49-year-old woman with a history of right-side abdomen pain for a few years. Diagnostic images revealed a large retroperitoneal cystic lesion. A laparoscopic resection was performed without spillage. The patient was discharged without complication postoperatively and no recurrence on follow-up. Surgical excision, either open/or laparoscopic without any spillage, remains the most effective and appropriate treatment for this lesion.
INTRODUCTION
Mixed serous and mucinous retroperitoneal cystadenoma is an extremely rare presentation as most of the cases reported in the literature are primary retroperitoneal mucinous cystadenomas (PRMC), with few being primary retroperitoneal serous cystadenomas (PRSC).
PRMCs are present with non-specific symptoms more frequently in women, and there is no established method found so far to diagnose it accurately. Once diagnosed, complete excision is recommended because of the risk of malignancy or degeneration or possible infection, even though it behaves in a benign fashion with no recurrences in most of the cases [1, 2].
There is a lack of epithelium in the retroperitoneum region, so PRSC is extremely uncommon. Very few case reports of this entity have been described in the literature. The pathogenesis of benign retroperitoneal cyst is not well understood [3].
As per our knowledge and literature search, there has been no case reported of benign retroperitoneal mixed serous and mucinous cystadenoma.
CASE PRESENTATION
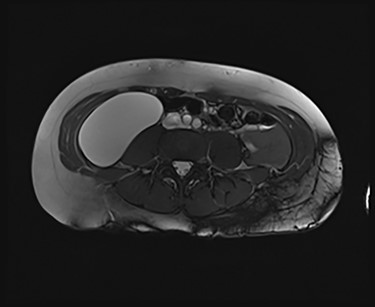
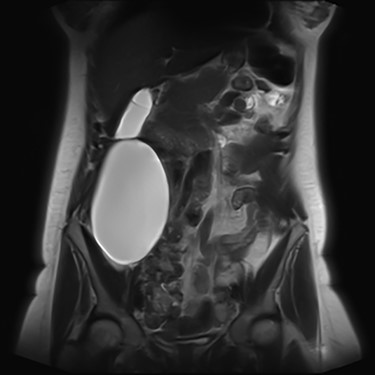
We present an extremely rare and isolated case of primary mixed serous and mucinous cystadenoma in a 49-year-old otherwise fit and healthy female patient. She was referred to our consultant with a history of discomfort on the right side of her abdomen for few years, which increased gradually with no other complains. The patient had further investigations conducted including computed tomography (CT) (Figs 1 and 2) that demonstrated the position and size of the lesion. The magnetic resonance imaging (MRI) revealed a large cystic lesion in the right retroperitoneal region shown in Figs 3 and 4. Her full blood count, inflammatory markers, urea and electrolytes and liver function tests were within the normal limit. Consequently, the patient had a laparoscopic resection of an isolated retroperitoneal cyst. At surgery, the cystic lesion seemed to be arising from mesentery and the lesion was dissected intact and completely excised. Histopathology revealed a benign mixed serous and mucinous cystadenoma as shown in Fig. 5. The patient was discharged from the hospital with no complications and fully recovered on follow-up review. Patient was discussed in a multidisciplinary team meeting and the recommendation was for no further management.


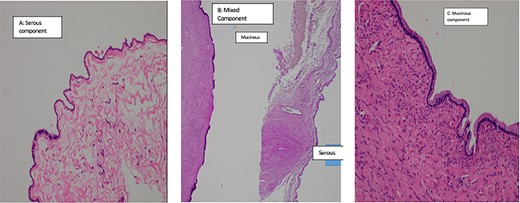
Histopathalogy slides of 47-year-old patient. (A) shows serous component. (B) shows mixed component. (C) shows mucinous component of the benign cyst.
DISCUSSION
Mixed retroperitoneal cystadenoma is extremely rare as mainly benign retroperitoneal adenomas are reported as PRMC or PRSC. A literature review failed to identify any reports of mixed PRMC and PRSC, and there are only three mixed pancreatic mucinous and serosal cystadenomas reported in the literature. One of the cases was treated with a laparoscopic central pancreatectomy with the patient making full recovery post-operatively [4–6].
Primary retroperitoneal cystic mucinous tumours are much more common than primary retroperitoneal cystic serous adenomas, although the exact contributing factors or underlying mechanisms remain unclear [7]. PRMC has been described as a rare tumour, since 1965 <100 cases have been reported. It is a cystic tumour, most commonly affecting females and has histological similarities with ovarian mucinous cystadenoma [8].
Based on a review of the cases reported in the literature, these tumours can be classified in three types. The most common type is the retroperitoneal mucinous cystadenoma. In the second type, the cells of the inner lining presents with foci of epithelial proliferation. This type resembles the ovarian mucinous cystadenomas of low malignant potential. The third type is the mucinous cystadenocarcinoma [9].
Primarily a PRMC presents as a painless mass with either pain and/or discomfort. Majority of the patients present with vague abdominal discomfort and asymptomatic mass. Its clinical presentation mainly depends on the location and the extent of the mass. Preoperative diagnosis is important, but this is difficult to achieve because no sensitive methods or reliable markers are available. Prompt diagnosis and management is required as most retroperitoneal masses are malignant [9].
Primary retroperitoneal serosal cystic lesions are uncommon heterogeneous clinical entities with no definite incidence [10]. The actual pathogenesis is not well understood, although one of the proposed hypotheses considers it to be an embryological remnant of the urogenital apparatus with epithelial and mesothelial tissues. These cysts oftentimes attain a very large size before becoming symptomatic [3].
Serological investigations are not helping with providing a definitive diagnosis. Tumour markers such as, carbohydrate antigen (CA) 19–9, CA 15–3, CA 125, carcinoembryonic antigen (CEA), alpha feta protein have not been shown to be sensitive or specific. Some cases demonstrated an increase in CEA and CA 19–9 in associated with PRMC. However, these are isolated case studies. With regard to radiological investigation, the ultrasonography lacks specificity [11]. Radiological imaging, such as MRI and CT, plays an important role in describing and assessing the disease’s characteristics and the involvement of adjacent or distant structures of the mass. None of the modalities can exclude the malignant potential of the retroperitoneal masses [9], as the diagnostic value of CT and MRI is similar [12]. Predominantly male patients and the patients who present with solid nodules in the cyst on their radiology images have strong association with malignancy [13].
Consistence with the literature, our patient presented with non-specific symptoms. Prompt diagnosis and treatment of the retroperitoneal lesion is important as the majority of retroperitoneal lesions could be malignant. As a final diagnosis of the disease is excision biopsy, and there is a possibility of malignancy, prompt action and excision of the cyst without spillage both laparoscopic and open is the treatment of choice.
In conclusion, mixed PRMC and PRSC is an extremely rare presentation, but it should be included in differential diagnosis of long-standing non-specific abdominal pain. Once a suspicion is raised, it should be taken seriously by prompt diagnosis and a complete surgical resection either open or a laparoscopic without spillage for complete recovery.
ACKNOWLEDGEMENT
Dr Tracey Lu, Pathologist, Histology and Cytology Department, Capital Pathology.
CONFLICT OF INTEREST STATEMENT
None declared.



