-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel G E Thiem, Bilal Al-Nawas, Peer W Kämmerer, Technical report and rare case description—patient-specific spacer made of bone cement for the revision of a PSI-TMJ fossa after screw fracture, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab466, https://doi.org/10.1093/jscr/rjab466
Close - Share Icon Share
Abstract
Total alloplastic temporomandibular joint replacement (TMJ-TJR) has once again become the focus of therapy for end-stage destroyed joints. Although material quality has increased significantly in terms of service life and wear, problems occur even with patient-specific (PSI) prostheses. Here, mainly the ramus components are affected and an occurrence of screw loosening or fractures in the area of the fossa of stock joints is rare and has not yet been described for patient-specific (PSI) components. Although very rare, such events pose a great challenge to both practitioners and affected patients, especially in the case of PSI components, not least due to the long time required for new fabrication. The case report shows a non-described screw fracture of a PSI-TMJ fossa and the first description of a temporary revision using a PSI-TMJ fossa made of bone cement.
INTRODUCTION
In recent years the use of alloplastic total temporomandibular joint replacement (TMJ-TJR) has emerged as a proven concept for the functional restoration of destroyed TMJs, but it still represents a challenge for surgeons. With the development of modern prosthetic materials, TMJ-TJR has once again become the focus of clinical application. However, according to the current consensus, it remains primarily reserved for TMJs that cannot be treated conservatively or with conventional surgical procedures or that can no longer be treated and have mostly undergone multiple operations and are severely damaged [1]. While the traditional alternative of autologous TMJ-TJR is almost exclusively associated with disadvantages and long-term complications, alloplastic reconstruction shows decisive advantages including a reduced duration of surgery and hospitalization, immediate loading, absence of donor-side morbidity, possible management of severely deformed joints and better predictability. Ankylosis, active condylar hyperplasia, joint-affecting tumor growth, previous TMJ operations (autologous and/or alloplastic TJR, other surgical interventions) and idiopathic condylar resorption are regular indications for TMJ-TJR. In view of increasingly early phases of TMJ disorders, the populations’ longer life expectancy and the desire for a higher quality of life, the indications for TMJ-TJR have been steadily increased and the timing of the procedure has been tending toward earlier intervention. In this context, female patients were shown to be predominantly affected (68%) and the age at procedure is significantly lower (40–50 years) compared with knee (~70 years) and hip (65 years) endoprosthetics [1].
CASE REPORT
This report is about a 63-year-old patient suffering of bilateral deforming TMJ arthrosis (Wilkes-V) from a bilateral condylar fracture. In 2019 he presented himself to the Department of Oral and Maxillofacial Surgery, showing painful palpation above both TMJs and a severely decreased mouth opening (maximum interincisal distance of 1.5 cm). A computed tomography (CT) scan then revealed pathognomonic changes with flattening of the condyle and articular eminentia as well as partial ankylosis of the right TMJ (Fig. 1). Based on these findings, we decided for a bilateral TMJ-TJR. At this point, the patient only wanted one side replaced for the time being. After impressions were taken, plaster models were 3D-surface scanned and in combination with the CT dataset further processed by Zimmer-BiometTM (Warsaw, USA) for patient-specific TJR (PSI-TJR) fabrication. Another 3 months later, the TMJ-TJR of the right side could be carried out (Fig. 2). Postoperatively the patient received antibiotics for overall 7 days. Satisfied with the result, the patient requested reconstruction of the left TMJ 6 months later. With an improved mouth opening (2.8 cm), impressions were taken using an intraoral scanner. After PSI fabrication, the operation was carried out 9 months after (Fig. 3). Six weeks following surgery, the patient presented with a painful preauricular swelling on the left side, which was diagnosed as aseptic inflammation in the absence of erythema and pathologic joint puncture. Showing a periarticular edema, a broken screw and radial osteolysis around the drilling channels, a subsequent CT scan indicated the loosening of the ultra-high-molecular-weight-polyethylene (UHMWPE) fossa component (Fig. 4). In view of the long production time of new custom-made components and the damaged implant site, we decided to explant the fossa and to temporarily replace it with a non-fixed patient-specific spacer made of COPAL®-bone-cement (Fig. 5) (gentamicin and clindamycin additive) (Haereus; Hanau, Germany). The workflow included the surface scan of the original fossa-drilling template, the computer-aided design of a two-part press mould and the intraoperative fossa fabrication from COPAL®-bone-cement. With the use of a rubber elastic intermaxillary fixation, the vertical mandibular relation could be secured, painful movements and muscle shortening avoided and the risk of perioperative infection could be sufficiently minimized (Fig. 6). After 3 months without complications, the patient-specific COPAL® component could be removed and the new patient-specific UHMWPE fossa inserted within sufficiently regenerated bone (Fig. 7).
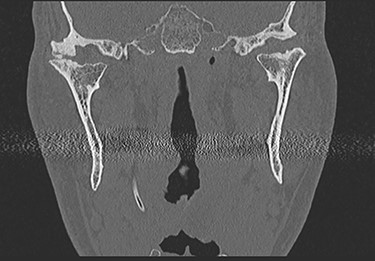
CT in coronal view with pathognomonic picture of deforming temporomandibular joint arthrosis on both sides.
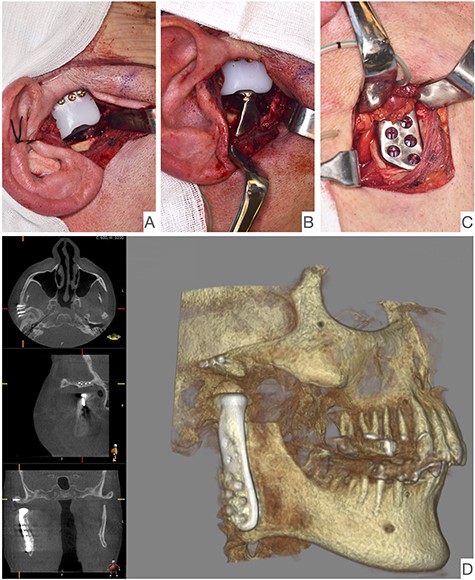
Intraoperative image showing the articular fossa (A) in combination with the articulating condylar component (B), the fixed ramus component (C) and the postoperative CBCT of the right side (D).
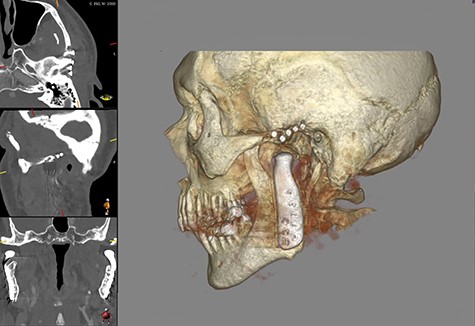
Shows postoperative CBCT after left TMJ replacement, 9 months after the right side.
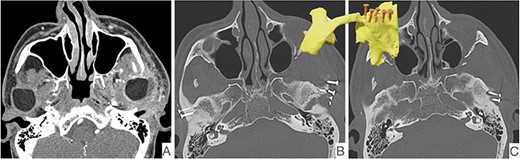
CT scan showing radiological signs of loosening of the left fossa component. On the left, the presentation of the periprosthetic edema (A), fracture of an osteosynthesis screw (B) and the osteolysis around the screw shafts (C).
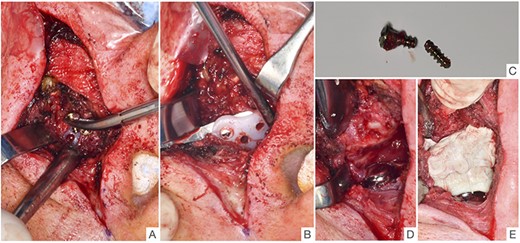
Intraoperative images show the removal of the loosened fossa component of the left side with removal of the shortened (broken) osteosynthesis screw (A), mobilization of the fossa component (B), the broken osteosynthesis screw (C), view of the condylar component (D) and condition after insertion of the patient-specific fossa component made of COPAL® bone cement (E).
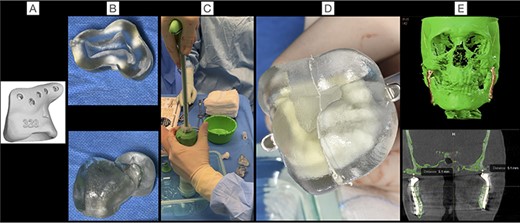
Shows the workflow to the PSI-COPAL®-TMJ fossa from the surface scan of the original fossa drill template (A), the creation of a two-part press mould (B), the intraoperative mixing of the bone cement (C), the shaping of the articular fossa (D) to the postoperative CT scan showing the symmetrical distance from condyle head to skull base on both sides (E).
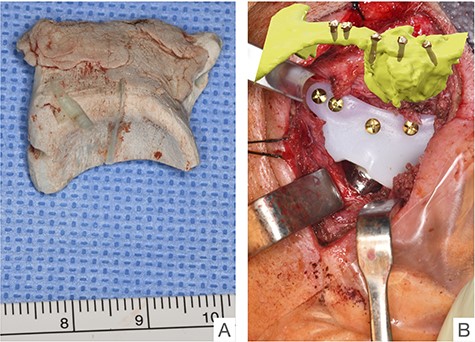
Condition of the PSI-COPAL®-TMJ fossa after explantation and situs after implantation of the newly fabricated UHMWPE articular fossa after healing of the bony implant site.
DISCUSSION
General complications regarding TMJ implants are periprosthetic infections, temporary or complete paresis of the facial and/or trigeminal nerve, swelling, bleeding, hematoma and material dislocation/failure [2–4]. In the past, complications occurred with the use of Proplast-Teflon implants, resulting in abrasion-induced foreign-body giant cell reactions with material intolerance, permanence and worsening of symptoms (pain, limited jaw mobility) as well as implant/material failure. By the use of wear-resistant materials (material combinations) such as UHMWPE for the fossa and cobalt–chromium–molybdenum or titanium alloy forming the condyle component, most of these disadvantages have been significantly reduced. The osteosynthesis screws used are made of titanium alloy by all well-known manufacturers [5]. And although current guidelines of European professional societies mention the risks of screw loosening and fracture, especially in the case of strong muscular hyperactivity [6], these events are extremely rare to not described at all in the literature for patient-specific/custom-made prostheses/implants [1, 5, 7]. PSI-TJRs are believed to allow less micromovement at the implant–bone interface due to their higher fitting accuracy based on high-resolution imaging techniques. This is in accordance with overall good long-term results described in the literature [8].
In this case report, all criteria of an aseptic material failure are applied, coming along with a painful swelling around the surgical site, absence of erythema, fever, oozing or a suppurating wound [9]. In contrast, early (<3 weeks) and late periprosthetic infections typically present signs of inflammation such as erythema, swelling, pain, fever and pus [10]. From our point of view, there are several reasons for the occurrence of the complication. The theory of occlusal malfunctions such as bruxism or pressing is one of them, but it is not supported either anamnestically or by grinding facets or other typical damage to the tooth structure. In addition, screw loosening can occur through thermal osteonecrosis caused by bone drilling with insufficient rinsing. Of course, this process cannot be ruled out by the authors, but it seems quite unlikely due to constant cooling of the drilling system and the additional application of irrigation fluid. Another reason could be the non-exact fit of the fossa component, which subsequently led to a loosening of the fossa component via micromovements with initial loosening and subsequent fracture of one of the fixation screws. The rare suspected diagnosis of PSI-TMJ-TJR failure (loosening/dislocation) was confirmed by a CT scan, showing osteolytic changes around the dislocated and fractured fixation screws of the fossa component. Thus, the present case met four of seven reasons to revise a failed TJR [11]. Since the fabrication of a new PSI took 10–12 weeks after design approval, given the acute clinical symptoms, we decided on the above-mentioned and ultimately successful procedure, including the fabrication of a patient-specific fossa component/spacer made of COPAL® bone cement. Since TJR revisions carry an increased risk for periprosthetic infections and the false negative rate of cases originally described as aseptic is 30% [12], we used an antibiotic-containing bone cement. To the best of our knowledge, this approach is the first to be described in the literature and, in conjunction with the extremely rarely described screw fracture in a PSI-TMJ fossa, represents an interesting case report for the professional community.
CONFLICT OF INTEREST STATEMENT
None declared.



