-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Asiri, Riyadh Alhedaithy, Zainab Alnazer, Cerebrospinal fluid leak post COVID-19 nasopharyngeal swab for a patient with idiopathic intracranial hypertension: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab456, https://doi.org/10.1093/jscr/rjab456
Close - Share Icon Share
Abstract
Coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2 is an infectious disease that led to a global pandemic. In this article, we reported a case of a young women who is known to have idiopathic intracranial hypertension, with iatrogenic skull base injury from a nasopharyngeal swab. Her case was complicated by meningitis.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an infectious disease that emergently led to a global pandemic. In attempts to control this pandemic, nasopharyngeal swabs to collect upper respiratory specimens are performed to diagnose and rule out infection. Real time-polymerase chain reaction of SARS-CoV-2 mRNA from the specimen is the primary diagnostic method around the world [1]. Although nasopharyngeal swab is considered a safe procedure, it has rare potential adverse effects. In this article, we reported a case of a young women who is known to have idiopathic intracranial hypertension (IIH), with iatrogenic skull base injury from a nasopharyngeal swab. Her case was complicated by meningitis.
CASE REPORT
A 36-year-old female patient presented to our emergency department with fever, headache, altered level of consciousness and agitation. Patient provided history of headache and clear watery rhinorrhea from the right side of the nose after nasopharyngeal swab for COVID-19 started four months prior to her presentation. She has a significant past medical history of IIH that was evident by magnetic resonance imaging (MRI) in 2018 with empty Sella Turcica sign (Fig. 1).
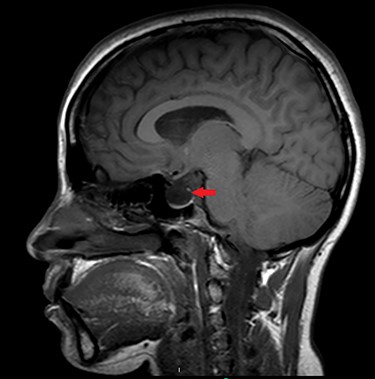
Sagittal MRI of brain, T1 weighted image, showing evidence of empty Sella Turcica (arrow).
Patient underwent sinus computed tomography (CT), which demonstrated opacification of the right sphenoid sinus (Fig. 2). Brain MRI showed possible cerebrospinal fluid (CSF) leak at the right sphenoid sinus (Fig. 3). Lumbar puncture was done and fluid sent for analysis to rule out meningitis.

CT of paranasal sinuses, showing opacification of right sphenoid sinus.

Coronal MRI of brain, T2 weighted image, showing opacification of right sphenoid sinus.
Fluid from nasal cavity collected and sent for β2-transferrin testing and confirmed to be positive for CSF.
Meningoencephalitis, likely bacterial, was diagnosed based on CSF results. The decision was made to start the patient on intravenous antibiotics. Patient progressed appropriately after the treatment and was discharged after thirteen days of admission. After that, the patient was followed in the clinic and improved with no more CSF rhinorrhea with conservative non-surgical management.
DISCUSSION
Nasopharyngeal swab has been used frequently to diagnose COVID-19 since the beginning of the pandemic. Inappropriate collection could lead to false-negative or false-positive results as well as transmission of the infection [1]. Little is written in the literature about adverse events. Cases of epistaxis, breakage of the swab into the nose, and CSF leak have been reported [2]. Leakage of CSF could be spontaneous, iatrogenic, or due to trauma. Iatrogenic causes account for about 16% of all CSF leaks. A very potential and serious complication of CSF leak that can be lethal is meningitis [3].
Two cases previously reported in the literature involved healthy patients who had CSF leak post COVID-19 nasopharyngeal swab due to injury of the skull base. One of the two cases was complicated by meningitis. Management involved surgical repair for one patient and conservative non-surgical management for the other [4, 5].
Two other reported cases of CSF leak post COVID-19 nasopharyngeal swab. Patients had, most likely, pre-existing unidentified encephalocele. It is believed that trauma to the pre-existing undiagnosed encephalocele led to the CSF leak. A medical history for one of the two cases was also significant for IIH and removal of nasal polyps over 20 prior to the presentation [6, 7].
In our case, iatrogenic CSF leak after the swab was identified in a patient with IIH. Her case was complicated with meningitis which resolved after intravenous antibiotics. However, underlying conditions that cause increase in intracranial pressure such as IIH could result in spontaneous CSF leaks [8, 9].
CONCLUSION
Patients with history of nasal surgeries and underlying pathologies and abnormalities might need special considerations and alternative diagnostic methods as they are at increased risk of serious adverse events.
Further education is necessary among healthcare providers about CSF rhinorrhea and associated symptoms to promote early diagnosis and treatment in order to avoid adverse complications like meningitis.



