-
PDF
- Split View
-
Views
-
Cite
Cite
Luca Cestino, Serena Mantova, Federico Festa, Giulia Carbonaro, Luca Dani, Alessia Fiore, Luca Bonatti, Stefania Soncini, Francesco Quaglino, Intestinal malrotation in one adult patient affected by SARS-CoV-2 infection: occlusion misdiagnosed as COVID gastroenteritis. Case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab451, https://doi.org/10.1093/jscr/rjab451
Close - Share Icon Share
Abstract
Malrotation of the gut is a rare occurrence, commonly diagnosed during childhood, but occasionally diagnosed in adults.
In children, intestinal obstruction is the most common manifestation, whereas in adult patients, the diagnosis is more challenging since the symptoms are less specific with several episodes of abdominal pain and vomit.
In a particular epidemic period, like the one we are going through, these generic symptoms may mislead to a wrong diagnosis.
We present the case of a young man in which occlusion due to intestinal malrotation has been misinterpreted as gastroenteric symptoms of severe acute respiratory syndrome coronavirus 2 infection, and we also overview the correct Ladd’s technique, commonly performed by pediatrical surgeon, but unusual operation for adult general surgeons.
INTRODUCTION
Malrotation of the gut is due to a failure of intestinal rotation during the embryogenic development, and it is associated to various complications commonly diagnosed in childhood: 90% of cases are discovered within the first year of life and 80% of these during the first month of life [1, 2]. According to some autopsy studies, the incidence is estimated around 1% of the population [3]. In adults, malrotation is rare and the incidence is around 0.19–0.2% [4–6].
During childhood, intestinal obstruction is the most common manifestation at the diagnosis, whereas in adults, the acute volvulus is discovered only in 10% of symptomatic patients and clinical presentation may be treacherous since adult patients commonly report prolonged history of intermittent abdominal pain, bloating and emesis, and the risk of complications is greater in adulthood [6, 7].
We report a case of subacute manifestation of intestinal malrotation in an adult affected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and misdiagnosed as a gastroenteritis coronavirus disease 2019 (COVID-19) related.
CASE REPORT
A 38-year-old male patient with neither known medical history nor former abdominal surgery was admitted to the emergency department with a 5-day history of abdominal pain associated with vomiting. He was hemodynamically stable and apyretic. The abdomen was moderately distended. Routine blood tests revealed only a mild electrolyte imbalance. Plain abdominal X-ray demonstrated a gastrectasia without significant bowel air-fluid levels (Fig. 1). A routine nasopharyngeal swab to detect SARS-CoV-2 infection with molecular real-time polymerase chain reaction test resulted positive. No respiratory symptoms or anomalies were discovered. The symptoms were referred to a gastroenteritis COVID-19 related and the patient was admitted to the Infectious Disease Hospital.
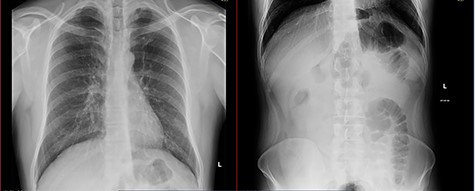
Two days later, for the persistence of symptoms, an abdomen computed tomography (CT) scan and surgical evaluation were required. The patient presented abdominal distension, tenderness without peritoneal signs, nausea and vomiting, but reported similar episodes auto-resolved abdominal in the past. The scan revealed a prominent gastrectasia, dilatation of duodenum and the first jejunal branch and jejunal mural edema was discovered, referable to an ischemic suffering, but there was no evidence of free air. The diagnosis was proximal bowel mechanical obstruction with suspect ischemic loop (Figs 2 and 3), so a surgical operation was proposed and the patients agreed.


The operatory room and the staff were prepared for a COVID patient according to Italian Surgical recommendations [7] and wore personal protective equipment, N98 FFP3 respiratory masks, suits, face shields and double gloves.
A midline laparotomy was performed: many adhesions and a few dilated jejunal loops were found, the duodenojejunal junction was uncommonly positioned on the right of the midline and on the right of the ascending colon, the cecum was in the upper central abdominal quadrant and was abnormally connected to the duodenum with ‘Ladd’s band’, causing the obstruction: the findings suggested intestinal malrotation. An extensive adhesiolysis and Ladd’s procedure, including a prophylactic appendectomy, were performed. There were no ischemic bowel loops, so no intestinal resection was needed.
The patient was admitted to a COVID department; bowel movements were present on 3rd postoperative day, but he was discharged on 15th postoperative day, when his SARS-CoV-2 nasopharyngeal swab resulted negative.
The preoperative CT was reviewed, considering intraoperative findings, and an incomplete bowel rotation was highlighted: duodenojejunal loop was abnormally located on the right side of abdomen and cecum was positioned at the left of mesentery, as illustrated in Fig. 2.
DISCUSSION
The symptoms presented by our patient were initially misinterpreted because of the concomitant presence of the SARS-CoV-2 infection. Gastrointestinal manifestations, represented by diarrhea, nausea, vomiting and anorexia, are predominant or exclusive in up to 17% of patients positive to SARS-CoV-2, as stated in a recent review [8].
Unlike in childhood, in adulthood, malrotations are discovered with a significant delay from the initial presentation [9]. According to the literature, the adult presentation is classifiable in acute and chronic. Chronic presentation is more common and is characterized by a range of unspecific symptoms, such as recurring and remitting abdominal pain, bloating, nausea and vomiting, often presenting since childhood [10, 11].
The adult malrotation is frequently discovered during surgery. Upper gastrointestinal (UGI) contrast study is considered the gold standard for the radiologic diagnosis of bowel malrotation in both pediatric and adult patients because of its sensitive and limited radiation exposure. UGI series are useful to evaluate the position of duodenojejunal junction, cecum and right colon and to reveal the presence of some typical malrotation signs like the bird’s beak sign of volvulus or the corkscrew appearance of the first jejunal loops [3]. The CT is widely used in the adults; it is useful to demonstrate the abnormal and inverted position of the superior mesenteric artery and the superior mesenteric vein or a typical twisted volvulus around the superior mesenteric artery (SMA) axis, described as whirlpool-like pattern loops [9, 12]. Moreover, the CT allows to identify suffering bowel loops.
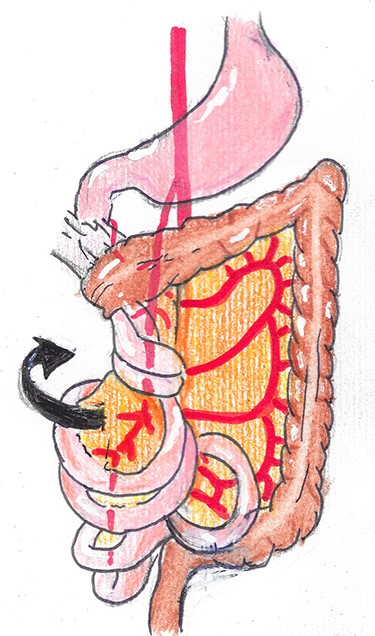
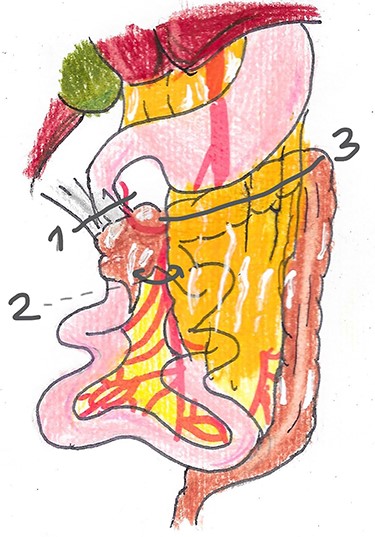
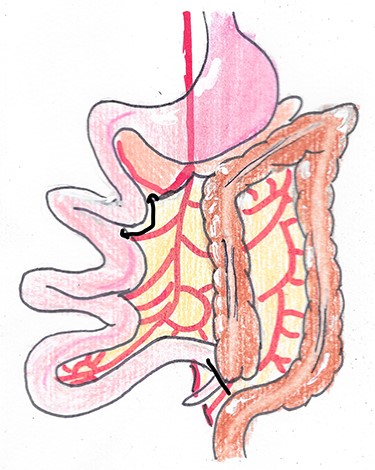
The treatment of malrotation is surgery, according to the open procedure described by Ladd in 1936 [13]. As claimed by current literature, surgical care of intestinal malrotation is indicated both in symptomatic patients and non-symptomatic patients in which the abnormality is incidentally discovered [3, 14]. Ladd’s procedure is a multistep surgical treatment, which consists in identification and counterclockwise detorsion of the volvulus, when present (Fig. 4), section of the Ladd’s bands, division of the adherences to enlarge the mesenteric root and prevent other volvulus (Fig. 5), and appendectomy (Fig. 6). At the end of the operation, the bowel is re-located in its normal position and suffering loops are eventually resected. Laparoscopic approach is accepted in the pediatric population and some studies suggest its feasibility and safety also for the treatment of adults [15].
Usually, general surgeons do not have experience with Ladd’s procedure. In a case series presented by Nehra and Goldstein [2], all child patients affected by intestinal malrotation underwent Ladd’s procedure, whereas in adult patients, malrotations were surgically treated exclusively in 61%, and only in 35% of them a correct Ladd’s procedure was carried out.
In conclusion, also adult general surgeons should know how to operate an intestinal malrotation, since this may be discovered during surgery, and we should keep in mind that, also in a pandemic period, SARS-CoV-2 infection may be only an occasional finding in a patient whose problem is due to a different cause.



