-
PDF
- Split View
-
Views
-
Cite
Cite
Junhui Jeong, Capillary hemangioma in the external auditory canal, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab445, https://doi.org/10.1093/jscr/rjab445
Close - Share Icon Share
Abstract
Hemangioma is a benign vascular soft tissue tumor. It is the most common soft tissue tumor in children and >60% of hemangiomas occur in the head and neck region. However, these tumors are rare in the external auditory canal (EAC). This case report describes a case of capillary hemangioma in the EAC in a woman 54 years of age. With the patient under local anesthesia in microscopic surgery, the mass was excised completely via a transcanal approach. If there is a cystic and pinkish mass in the EAC with symptoms of bleeding or pulsatile tinnitus, hemangioma should be considered. For symptomatic hemangioma, complete surgical excision is necessary and the prognosis is good after excision. Histopathologic confirmation is mandatory after excision.
INTRODUCTION
Hemangioma is a benign vascular soft tissue tumor [1–4]. It is the most common soft tissue tumor in children and >60% of hemangiomas occur in the head and neck region. However, these tumors are rare in the external auditory canal (EAC) [4]. In spite of its rarity, hemangioma in the EAC can be associated with symptoms, which can bring a patient to the clinic. This case report describes a rare case of capillary hemangioma in the EAC in a woman 54 years of age.
CASE REPORT
A 54-year-old woman visited our otorhinolaryngology clinic for a cystic mass in the left EAC with intermittent bleeding for several years. On physical examination, a 0.6 × 0.6 cm, soft, pinkish, cystic mass was observed in the posterior cartilaginous portion of the left EAC (Fig. 1). Facial computed tomography (CT) revealed an enhanced cystic mass in the posterior cartilaginous portion of the left EAC (Fig. 2). Considering a vascular tumor, surgical excision was planned because the patient had intermittent symptoms of bleeding.
With the patient under local anesthesia in microscopic surgery, the mass was excised completely via a transcanal approach. Bleeding was not massive. After excision, the skin defect was minimal. Histopathologic examination revealed a proliferation of dilated capillary-sized vessels with surrounding fibrous stroma. Thus, capillary hemangioma was diagnosed. After surgery, symptom of intermittent bleeding in the left EAC improved. The patient had no complications and there was no recurrence after two years and six months.
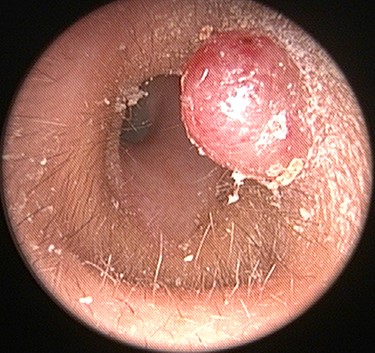
A 0.6 × 0.6 cm, soft, pinkish, cystic mass in the posterior cartilaginous portion of the left external auditory canal.
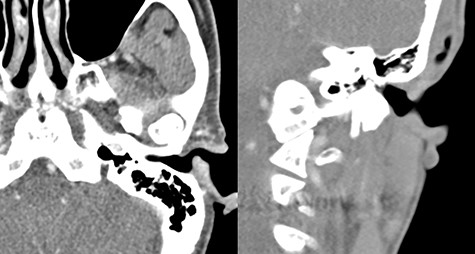
Facial CT revealing an enhanced cystic mass in the posterior cartilaginous portion of the left external auditory canal. (A) Axial view and (B) coronal view.
DISCUSSION
In 1982, Mulliken and Glowacki presented a classification of vascular tumors into two categories, hemangiomas and vascular malformations [2, 4–6]. Hemangioma is a common vascular tumor that has an increased number of vessels filled with blood [4, 6]. In contrast, a vascular malformation such as arteriovenous malformation is composed of vascular channels with flat mature endothelium [5]. The incidence of hemangioma is 1–2.6% at birth and 10% in 1-year-old children. Half of hemangiomas regress spontaneously within 5 years old and the rest usually regress by 10–12 years old [1, 4].
Histopathologically, hemangioma is classified into capillary hemangioma, cavernous hemangioma and mixed hemangioma. Cavernous hemangiomas are composed of large cavernous vascular spaces and present after the sixth decade of life [2, 4]. In contrast, capillary hemangiomas have capillary-like channels with surrounding fibrous stroma that result from endothelial proliferation [2, 3, 6]. These present in infants and regress spontaneously before 5 or 6 years of age [2–4]. Both cavernous and capillary hemangiomas in the EAC are rare [1–4, 6], and in adults fewer cases of capillary hemangioma have been reported compared to those of cavernous hemangioma in the EAC.
Hemangioma occurs in two developmental stages, which are a quick growth stage (proliferative stage) and a decline stage. Histopathologically, there is endothelial hyperplasia and an increase in mast cells in the proliferative stage, whereas there are fibrosis, infiltration of fat, cell reduction and normalization of mast cells in the decline stage [2].
Hemangioma in the EAC may present with no symptoms, but symptoms such as bloody otorrhea, hearing loss, aural fullness and pulsatile tinnitus can occur if the mass is large [1, 3, 4]. Radiological evaluations such as CT and magnetic resonance imaging are useful in vascular tumors [2]. CT is the best choice as the diagnostic imaging tool [4]. It provides tumor size and extent [1, 2].
If the mass does not induce symptoms, treatment is not necessary and observation is reasonable. For the symptomatic mass, the treatment of choice is complete surgical excision [2–4, 6]. Other treatments that include embolization, mastoidectomy or radiation may be considered [3]. Preoperative angiography and embolization is usually unnecessary unless massive bleeding is expected [3, 4]. Hemangioma should be differentiated from glomus tumor, aural polyp, arteriovenous malformation, attic cholesteatoma and carcinoma [1, 2, 4].
Definite diagnosis is possible by histopathologic evaluation, thus histopathologic confirmation is necessary after surgical excision. Sometimes, it is difficult to differentiate capillary hemangioma from pyogenic granuloma, which is also called lobular capillary hemangioma. Both of these have the histologic similarities of capillary hemangioma [7]. However, pyogenic granuloma shows proliferation in lobules and predominant perithelial characteristics, rather than endothelial characteristics [7, 8].
If there is a cystic and pinkish mass in the EAC with symptoms of bleeding or pulsatile tinnitus, hemangioma should be considered. For symptomatic hemangioma, complete surgical excision is necessary and the prognosis is good after excision. Histopathologic confirmation is mandatory after excision. Capillary hemangioma may also be revealed in the EAC in adults as a cavernous hemangioma.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This case report did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
ETHICAL APPROVAL
The Institutional Review Board of the National Health Insurance Service Ilsan Hospital exempted the review of this study (NHIMC 2020-12-018).



