-
PDF
- Split View
-
Views
-
Cite
Cite
Matías Ezequiel La Francesca, Carolina López, María Sol Kraiñski, Fiorela Hanndorf, Mariano Laporte, Postoperative chylous leak after a laparoscopic low anterior resection: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab443, https://doi.org/10.1093/jscr/rjab443
Close - Share Icon Share
Abstract
Chylous leakage is an unusual event after abdominal surgery and even more during colorectal procedures. The management of this complication is already discussed in medical literature. In our case a laparoscopic low anterior resection to an 81-year-old woman with a sigmoid and rectum colon tumor was done. The fourth day after surgery postoperative chylous leakage was diagnosed. It was treated with suspension of oral feeding, total parenteral nutrition and Octreotide with a favorable resolution.
Chylous leakage is a type of postoperative lymphatic leakage that occurs when chyle fluid drains from the drainage tube without evidence of lymphocele, lymphorrhea or chylous ascites [1]. Chylous leakage after a colorectal surgery is an unusual incident with an incidence of 2.8% after an anterior resection [2].
There is no agreement in medical practice guidelines about its treatment.
This is a successful case of conservative management of this complication.
An 81-year-old woman without history of other diseases presented with abdominal pain, weight loss and altered bowel habit for 3 months. Colonoscopy informed a 10-cm tumor from 20 to 30 cm from the anal verge. Abdominal and pelvis CT scan (computed tomography) showed a circumferential thickening in sigmoid rectum and colon.
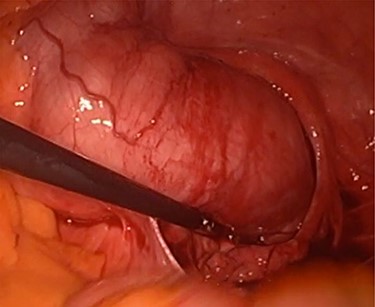
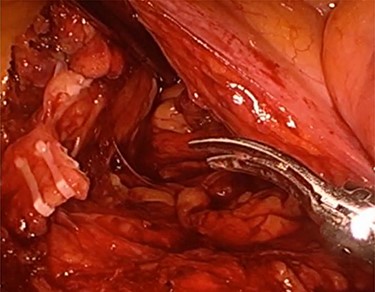
A laparoscopic low anterior resection, colorectal anastomosis with protective colostomy was performed (Fig. 1). The procedure was completed using advanced bipolar cautery to dissect tissues and hemoclips to ligate vascular vessels (Figs 2 and 3), the colorectal anastomosis was done 4 cm from de anal verge using a circular stapler and a pelvic drainage tube was placed. The operating time was 190 min without need of blood transfusion.
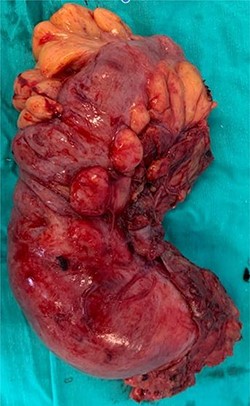
Postoperative pathological anatomy informed a well differentiated sigmoid colon and superior-middle rectum adenocarcinoma (GH1, N2 and M1), 14 lymphatic nodes were isolated without evidence of metastasis (0/14).
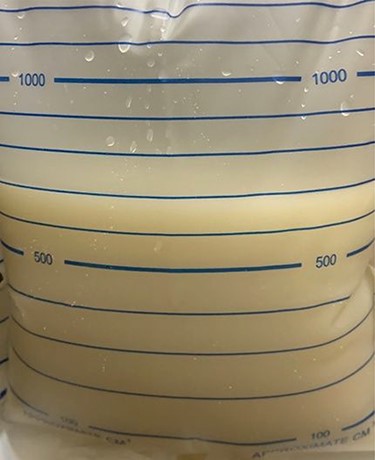
The patient passed immediate postoperative in intensive care unit and the day after returned to a sickroom and started oral feeding without complications until the fourth postoperative day when the pelvic drainage developed a milky and cloudy fluid. At first no therapeutic changes were implemented, however 24 h later the abdominal drainage collected 500 ml of that fluid, which was biochemically analyzed obtaining 1479 mg/dl of triglycerides, making diagnosis of postoperative chylous leak (Fig. 4).
The patient was asymptomatic without abdominal pain, bowel habit was conserved, no changes in laboratory tests were found and an abdominal ultrasound was requested without evidence of free fluid or abdominal collections. Therefore, together with nutritionists staff, a high protein, low fat with medium chain triglyceride (MCT) diet was implemented, but no clinical changes were observed, even the amount of fluid increased during the next 48 h, reaching 1000 ml per day at the eighth postoperative day.
For this reason, our group decided to take more aggressive therapeutic measures, oral feeding was suspended, and a central venous catheter was placed, starting total parenteral nutrition (NPT) with the subcutaneous administration of Octreotide 0.1 mg every 8 h. During the first 48 h of treatment the amount of fluid did not change but its characteristics did, it became more serous. The quantity of fluid started to decrease during the next 24 h, and 72 h later it was <100 ml per day. Then NPT was gradually suspended, restarting at the same time oral feeding.
At the 16th postoperative day a new abdominal ultrasound demonstrated no complications, the abdominal drainage was retired and the patient discharged from the hospital with a high protein, low fat with MCT diet for 1 month. She continued with periodic controls without relapses.
There are very few report cases of lymphatic leakage after a colorectal surgery, it is thought that the injury mechanism is caused by the disruption of lymphatic channels during the vascular control near paraaortic area [3]. The risk of overlooked injuries is greater during laparoscopic procedures because of CO2 pressure over lymphatic channels [4]. In this case, the permanence of the abdominal drainage prevented the development of chylous ascites with its nutritional and infectious complications.
There is no agreement in literature about the management of this complication but it seems suitable begin with a conservative treatment instead of surgery.
Although conservative management is feasible, its effectiveness has been variable, from 77 to 100% of success in previous studies [5]. Different approaches involve the concept ‘conservative’; a high protein, low fat supplemented with MCT, enteral nutrition (EN) or NPT. MCT are absorbed into the intestine and transported to the portal venous system reducing the production of chyle. The use of diet on its own does not need hospitalization but usually is not well tolerated by patients and may be insufficient. NPT and EN with MCT have showed to be equally effective in terms of days needed to reduce drainage volume and length of hospital stay but NPT has the disadvantage of requiring hospitalization and a central venous catheter with its related complications [6]. In our case the use of NPT was chosen because an EN free lipid formulation was not available. The association of medical therapy with dietary measures improves the favorable outcomes [6]. Somatostatin suppress glucagon effects and reduce the chyle flow, its synthetic equivalent, Octreotide has similar effects with the advantage of a lower cost and longer half-life which allows subcutaneous administration.
Recently, a case of chylous ascites successfully treated using lymphangiography and embolization with lipiodol was published and may be a promising strategy for cases in which conservative management is not enough [7].
Surgery should be considered after 6–8 weeks of unsuccessful conservative treatment, surgical repair of the leakage using direct suture, ligation or fibrin glue have been reported, unfortunately the exact leakage site due to the inconstant lymphatic anatomy is not frequently located causing additional harm without benefits [8].
This report case of a chylous leakage successfully treated with Octreotide and NPT emphasizes the importance of prevent this complication with a meticulous dissection during the surgery and If it is not possible treat it through a conservative management leaving surgical reintervention as the last option.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient prior to publication.



