-
PDF
- Split View
-
Views
-
Cite
Cite
Tharindu Senanayake, Imran Kader, Ferdinand Miteff, Arvind Deshpande, Common carotid to vertebral artery bypass to facilitate endovascular treatment of a basilar artery aneurysm, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa579, https://doi.org/10.1093/jscr/rjaa579
Close - Share Icon Share
Abstract
Large posterior circulation intracranial aneurysms have a high risk of significant morbidity or mortality if left unmanaged. Endovascular techniques are well established as primary treatment for such aneurysms. This includes placement of endovascular flow diversion stents that result in progressive thrombosis and resolution of aneurysms. Successful stent placement is reliant on suitable cervical vascular access. We report a case of a 60-year-old male without direct vertebral artery access to a fusiform basilar artery aneurysm. Successful endovascular treatment required a novel hybrid technique utilizing a right common carotid to V3 segment vertebral arterial bypass to gain endovascular access to the aneurysm.
INTRODUCTION
Large posterior circulation intracranial aneurysms have a high risk of significant morbidity or mortality if left untreated [1]. The mainstay of management of these aneurysms is through the use of endovascular techniques due to a significant reduction in procedural complications compared to open aneurysm clipping. A commonly used endovascular technique is use of a flow diversion stent, which aims to alter the local blood flow with the aim of leading to thrombosis within the aneurysm sac whilst allowing distal vessel flow [2]. However, a prerequisite for this is presence of suitable vascular anatomy to allow access to the aneurysm [3]. The following case describes the dilemma associated with inadequate access to a fusiform basilar artery aneurysm and the use of a hybrid technique to gain endovascular access.
CASE REPORT
A 60-year-old male initially presented for investigation of headaches and underwent a contrast enhanced computed tomography scan of his brain. The scan revealed a 20 mm × 10 mm basilar artery aneurysm that was deemed not surgically operable (Fig. 1). Such an aneurysm carries an 18.4% 5-year rupture risk [4]. His past medical history included coronary artery disease, atrial fibrillation, a metallic mitral valve, a prior ischaemic stroke, hypertension and a previous provoked deep vein thrombosis. He was otherwise a functionally independent, relatively young man with an incidental but high-risk aneurysm that required treatment. Anatomically, his left vertebral artery terminated in the posterior inferior cerebellar artery (PICA) and did not communicate with the aneurysm. The right vertebral artery was occluded at its origin and reconstituted via collaterals from the right thyrocervical trunk at the V3 segment. Attributable to significant tortuosity of this vessel, the initial attempt at stenting the aneurysm was unsuccessful.
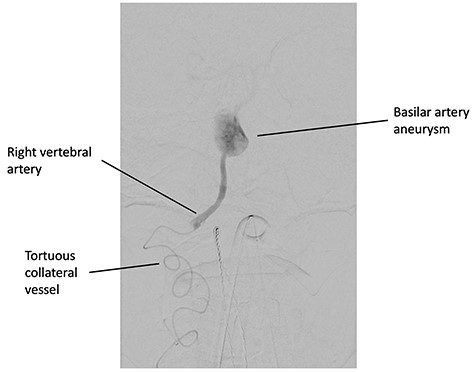
Digital subtraction angiography, demonstrating the catheter in the tortuous collateral vessel from the right thyrocervical artery supplying the right vertebral artery.
To allow endovascular access to the aneurysm, the patient underwent a right CCVAB. The procedure was performed under general anaesthetic with nasotracheal intubation. The mid portion of the right common carotid artery (CCA) was exposed in the neck above the omohyoid muscle via a longitudinal incision anterior to the medial border of the sternocleidomastoid. The incision was extended cranially and posteriorly to behind the ear and the extradural V3 segment of the vertebral artery was exposed between the transverse processes of C1 and C2. The long saphenous vein was harvested from the left thigh, reversed and after systemic heparinization, anastomosed in an end to side fashion to the CCA and to the vertebral artery. A contrast enhanced computed tomography scan confirmed patency of the graft on the Day 1 post procedure (Fig. 2). In the early post-operative period, the patient had ongoing hypotension that was likely secondary to cerebral autoregulation of blood pressure post CCVAB. The patient had also suffered from a line sepsis, which delayed the second stage of the operation.
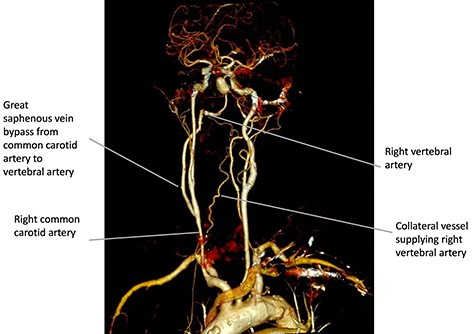
Three-dimensional reconstruction of the contrast enhanced computed tomography scan performed on Day 1 post CCVAB, demonstrating a patent bypass and flow through the right vertebral artery and to the aneurysm.
Six weeks after the bypass procedure, the patient underwent an angiogram from the right common femoral artery (Fig. 3). Access to the basilar artery aneurysm was achieved via a coaxial system consisting of a 6F long sheath to the origin of the anastomosis, a 5F intermediate guide within the graft and a 025 microcatheter to deliver a 3 × 35 mm flow diverting Pipeline stent (Medtronic, California, USA) to exclude the basilar artery aneurysm. There were no significant complications and the patient recovered well.
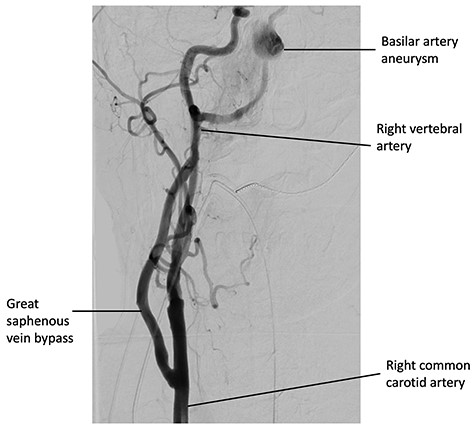
Digital subtraction angiography from the right common carotid artery, demonstrating the CCVAB and decreased filling of the basilar artery after a successful delivery of the pipeline flow diverting stent.
DISCUSSION
Basilar artery aneurysm rupture is associated with significant morbidity and mortality and can pose difficult management decisions [1]. The two main contemporary management options are microsurgical clipping or endovascular stenting of the aneurysm. Due to lower rates of morbidity and mortality, the first-line management is an endovascular approach [5].
CCVAB is an uncommonly performed extracranial bypass procedure that is normally indicated for the management of recurrent posterior circulation ischaemic events or vertebrobasilar insufficiency and can be an effective procedure in those circumstances [1]. The use of an extracranial bypass for the purpose of allowing endovascular access to the posterior circulation for treatment of an aneurysm is exceptionally rare, being described in only one other single small case series internationally [3]. This case demonstrates that CCVAB provides a viable hybrid management approach in complex cases.
Patients with hostile anatomy pose technical challenges in endovascular surgery. Vertebral artery anatomical variants and proximal atherosclerotic vertebral artery occlusive disease are common [6]. Notable variants include vertebral artery duplications, unilateral hypoplasia and termination in the PICA [7]. Whilst it is difficult to accurately estimate the population prevalence of vertebral artery termination in the PICA, it may be between 2–18.7% [7, 8].
CCVAB carries a number of procedural risks including stroke and bypass occlusion but is a safe and durable procedure in experienced hands. For the patient presented in the case, open neurosurgical clipping was deemed not an option due to technical considerations and his only option was endovascular therapy. Nonetheless, the risks of total morbidity and mortality in open clipping are thought to be higher compared to endovascular therapy, especially for large posterior circulation aneurysms [4]. Furthermore, a conservative approach was undesirable due to the high risk of rupture. The surgical exposure required for CCVAB was a low approach in the anterior neck since the distal internal carotid artery was not exposed. This approach may require transection of the transverse cervical nerves leading to numbness of the anterior neck. Levator scapulae and splenius cervicis were divided, but this is well tolerated post-operatively. Key structures at risk include the vagus nerve, accessory nerve and the ramus of the C2 spinal nerve. In our case, the sternocleidomastoid muscle was left intact and reflected to allow anastomosis of the vessel. A low approach minimizes the potential morbidity associated with division of the digastric muscle, resection of the styloid process, subluxation of the mandible or mobilization of the hypoglossal nerve.
The optimal timing for endovascular treatment post bypass has not been definitively established. In institutions that lack hybrid facilities, a staged procedure can be safely performed. Due to the novelty of this procedure, it is difficult to ascertain whether there is increased risk of aneurysmal rupture following CCVAB. This potential risk was controlled post-operatively with strict blood pressure monitoring to aim for normotension. In hybrid facilities, concurrent therapy with endovascular therapy after the creation of the CCVAB could be possible. Whilst direct CCA puncture could theoretically be performed to avoid aortic arch wire manipulation, this is undesirable when the bypass is anastomosed to the proximal CCA. In our patient, there would have been minimal safe distance to insert a sheath below the bypass without a sternotomy [9]. Due to these reasons, it was deemed safer to gain access from the groin and negotiate the aortic arch.
This case demonstrates that CCVAB is a safe and feasible option to allow endovascular access for stent placement to treat complex posterior circulation aneurysms with unsuitable endovascular access.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



