-
PDF
- Split View
-
Views
-
Cite
Cite
Andy Chao Hsuan Lee, Francis J Podbielski, Infected port-a-cath leading to subpectoral and sterno-manubrial abscess, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa576, https://doi.org/10.1093/jscr/rjaa576
Close - Share Icon Share
Abstract
Sterno-manubrium and subpectoral abscess have been rarely reported in literature. If the diagnosis and treatment are not properly performed, a soft tissue abscess can cause serious complications such as sepsis or even death. Therefore, awareness of such conditions is essential for early diagnosis and prompt treatment. Here, we report a case of sterno-manubrial and subpectoral abscess with significant destruction of cartilage due to extension from an infected subclavian porta-a-cath. Our management started with intravenous antibiotic therapy initially; however, due to lack of clinical resolution, incision and drainage followed by serial debridements were performed, highlighting importance of awareness of uncommon presentation.
INTRODUCTION
There have been very few case reports regarding subpectoral chest abscess and sterno-manubrial abscess. Because this form of localized suppuration is unfamiliar to many physicians, tendencies have been to treat conservatively for long periods [1]. Surgery is generally the treatment of choice for abscess, but occurs frequently after the process has spread widely, with extensive tissue destruction [2]. Here, we report a case of sterno-manubrial and subpectoral abscess due to direct extension of infection from an infected central venous catheter.
CASE REPORT
A 59-year-old male with history of metastatic prostate cancer who was undergoing chemotherapy via right subclavian port-a-cath developed catheter-associated infection with erosion of catheter through the skin. The catheter was removed and the wound left open to allow healing by secondary intention. The patient did well initially; however, 6 weeks later, he developed fullness and pain worsened with movement over the area of sterno-manubrial joint, which prompted further evaluation. Upon presentation, patient was afebrile and hemodynamically stable. Patient had leukocyte count of 7260/mm [3]. Patient was found to have a warm, dry, 3.5 cm area of fluctuance and mild overlying erythema at sterno-manubrial joint, with minimal tenderness to palpation. Computed tomography scan of chest showed 1.8 × 2.8 × 3.6 cm fluid at right subpectoral space and sterno-manubrial joint (Fig. 1). Given the seemingly small size of the abscess, medicine service pursued conservative management with empiric intravenous vancomycin initially, which was later de-escalated to intravenous cefazolin after abscess aspirate culture grew methicillin-sensitive Staphylococcus aureus. After 5 days, however, there was no sign of resolution of the sterno-manubrial fluctuance. The thoracic surgery service was consulted, whose initial impression was that the recent catheter-associated infection had tracked from the old port pocket to the cartilage between the sternum and the rib, causing significant destruction of cartilage and subcutaneous abscess formation. Patient was taken to operating room for incision, drainage and debridement of the right subpectoral space and sterno-manubrial joint abscess (Fig. 2). Patient underwent three additional serial debridements and wound wash-outs every other day. During each debridement, the wound was generously debrided using curette and low-setting cautery with excision of portion of subpectoral fascia and portion of cartilage from sterno-manubrial joint space. Bony structures remain grossly intact with no sterno-manubrial joint instability. The abscess cavity was copiously irrigated and packed with silver sulfadiazine-impregnated half-inch packing gauze. Intraoperative culture grew S. aureus that was resistant only to penicillin. Histopathology study from intraoperative samples showed tissue necrosis with accompanying marked acute inflammation, abscess formation and small fragments of benign bone. In his fourth serial debridement operation, there was adequate healthy granulation tissue present at which point wound closure was performed and a Jackson Pratt drain was placed. Patient was discharged home with additional 8 weeks of intravenous cefazolin treatment. At follow-up in thoracic surgery clinic 2 weeks later, patient’s incision had healed well with no signs of residual infection. Jackson Pratt drain was removed.
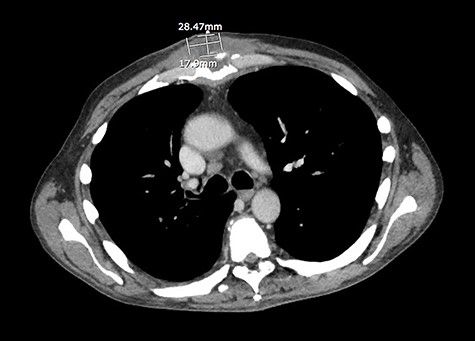
CT scan of the chest revealed a 1.8 × 2.8 × 3.6 cm fluid at right subpectoral space and sterno-manubrial joint.
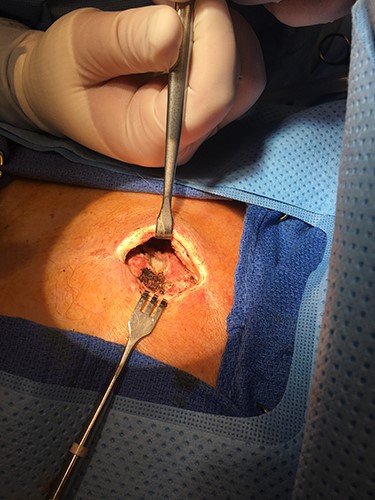
Incision, drainage and debridement of the right subpectoral space and sterno-manubrial joint abscess.
DISCUSSION
Given that there has been no case report on sternal or subpectoral infection secondary to contiguous infection from an infected central venous catheter, the work up and management of such disease process may need to be extrapolated from other more common secondary sternal or subpectoral infections. Subpectoral abscess is reportedly associated with previous injury in the upper extremity [3]. The essential pathology in this condition has been described as bacteria draining through lymphatic vessels from the primary focus [2]. Demonstrable fluctuation is regarded as a late and uncertain manifestation of this syndrome. Early incision and drainage, which provide the treatment of choice, prevent the extension of the suppurative process to other regions and bring about rapid subsidence of the infection [2]. Due to unfamiliarity of the disease presentation and management, tendencies have been to treat expectantly and conservatively for relatively long periods, which subject patient to a painful course of several days or weeks’ duration [2].
Our patient had no prior upper extremity trauma; however, an infected porta-catheter may serve as the primary focus from which bacteria drained through lymphatics and reached the subpectoral space, eventually eroding the cartilage of sterno-manubrium joint and forming an abscess. A patient actively receiving chemotherapy is at increased risk for infection. Our patient did not look acutely ill during our initial evaluation; however, he had very significant localized signs on physical examination. The timely recognition of failure of conservative treatment led us to operative management, which quickly controlled the infection.
Instituting strategies against implantable venous access port infection might have been the best method for prevention of this rare complication. Maximum sterile barrier precautions, including gloves, cap, mask, gown and full-body drape, and proper skin preparation should be followed during catheter insertion [4]. After insertion, training of patients, nursing teams and physicians in handling port-a-cath is mandatory to minimize the risk of bacterial contamination [5]. Proper Huber needle usage and proper sterile barrier and skin preparation during each port access should be strictly followed [4].
A review of the literature for similar cases using key words ‘subpectoral abscess’ yielded only seven case reports and case series since 1928, none of which was associated with ‘central venous catheter’. However, with timely recognition through clinical evaluation, accurate early imaging diagnosis, and prompt definitive treatment, resolution of symptoms of this life-threatening infection can be achieved.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



