-
PDF
- Split View
-
Views
-
Cite
Cite
Simone Celotti, Laura Benuzzi, Chiara Ceriani, Piero D’Amore, Diego Foschi, Luca del Re, Laparoscopy management for spontaneous bladder rupture: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa570, https://doi.org/10.1093/jscr/rjaa570
Close - Share Icon Share
Abstract
We present a case of a 79-year-old man with lower abdominal pain and negative Blumberg sign. An indwelling bladder catheter was inserted for urinary retention due to a tight phimosis 2 months earlier. A contrast-enhanced computed tomography scan revealed a huge gastrectasia and small bowel distention due to a suspected adherent bridle. The clinical signs and the laboratory tests were highly suspicious for bowel obstruction and emergency surgery was indicated. Exploratory laparoscopy showed a bladder hole tamponade by an ileum loop. The perforation was sutured laparoscopically and the patient was discharged on the 14th postoperative day. In our case, emergency laparoscopic exploration was useful for the diagnosis and the treatment of spontaneous bladder rupture. We hope this case report can be useful to give these patients better outcomes. Notably we would like to emphasize that the presence of a urinary catheter can be a risk factor for intraperitoneal bladder rupture.
INTRODUCTION
Spontaneous bladder rupture is a rare and life-threatening event. The most common risk factors are chronic inflammation such as infections or irradiation, urinary retention due to outflow obstruction or neurogenic bladder, and malignancies [1, 2]. In these conditions, the development of bladder diverticula is easier. Bladder diverticula are bulging sacs from weakness points on the bladder wall with a higher risk of perforation. The most frequent sites of diverticulum perforation described in the literature are intraperitoneal: bladder dome or posterior wall [1].
Patients with intraperitoneal bladder rupture present with symptoms and signs of acute abdomen and the perforation is often initially misdiagnosed even with the aid of computed tomography (CT) scans. A multidetector CT cystography is the gold standard for suspected bladder rupture evaluation [3]. Once the diagnosis is established, the management of spontaneous bladder rupture can be either non-operatively or surgical. Surgery is indicated for intraperitoneal ruptures [4]. The objective of this case report is to highlight the role of emergency laparoscopic exploration.
CASE REPORT
A 79-year-old man was referred to our Emergency Department (ED) for abdominal pain since morning without other symptoms. His medical history consisted of Parkinson’s disease and recent onset of Alzheimer’s disease. Bilateral hydronephrosis secondary of a tight phimosis occurred 2 months earlier. An indwelling bladder catheter was inserted for urinary retention and routinely changed. The patient had not prior surgical history.
His vital signs were blood pressure 115/60 mmHg, rhythmic pulse rate of 99 beats per minute, oxygen saturation 94% on room air and body temperature of 37.1°C. His urine output was 80 ml/h by a well-functioning catheter.
The physical examination showed a painful distended abdomen especially in the lower quadrants with a weak peristalsis and negative Blumberg sign. Laboratory analysis showed elevated white blood cells count and C-reactive protein (Table 1).
| Blood test . | . | Hemogasanalisis . | . |
|---|---|---|---|
| Leukocytes (×109/l) | 16.05 | pCO2 (mmHg) | 25.8 |
| Hemoglobin (g/dl) | 12.1 | pO2 (mmHg) | 71.4 |
| Platelets (×109/l) | 188 | BE (mmol/l) | -5.6 |
| C-Proteine Reactive (mg/dl) | >7 | HCO3- (mmol/l) | 17 |
| Creatinine (mg/dl) | 1.3 | Lactate (mmol/l) | 1.10 |
| PT-ratio (INR) | 1.26 | Sodium (mmol/l) | 145.8 |
| PTT-ratio | 1.10 | Potassium (mmol/l) | 3.29 |
| Blood test . | . | Hemogasanalisis . | . |
|---|---|---|---|
| Leukocytes (×109/l) | 16.05 | pCO2 (mmHg) | 25.8 |
| Hemoglobin (g/dl) | 12.1 | pO2 (mmHg) | 71.4 |
| Platelets (×109/l) | 188 | BE (mmol/l) | -5.6 |
| C-Proteine Reactive (mg/dl) | >7 | HCO3- (mmol/l) | 17 |
| Creatinine (mg/dl) | 1.3 | Lactate (mmol/l) | 1.10 |
| PT-ratio (INR) | 1.26 | Sodium (mmol/l) | 145.8 |
| PTT-ratio | 1.10 | Potassium (mmol/l) | 3.29 |
| Blood test . | . | Hemogasanalisis . | . |
|---|---|---|---|
| Leukocytes (×109/l) | 16.05 | pCO2 (mmHg) | 25.8 |
| Hemoglobin (g/dl) | 12.1 | pO2 (mmHg) | 71.4 |
| Platelets (×109/l) | 188 | BE (mmol/l) | -5.6 |
| C-Proteine Reactive (mg/dl) | >7 | HCO3- (mmol/l) | 17 |
| Creatinine (mg/dl) | 1.3 | Lactate (mmol/l) | 1.10 |
| PT-ratio (INR) | 1.26 | Sodium (mmol/l) | 145.8 |
| PTT-ratio | 1.10 | Potassium (mmol/l) | 3.29 |
| Blood test . | . | Hemogasanalisis . | . |
|---|---|---|---|
| Leukocytes (×109/l) | 16.05 | pCO2 (mmHg) | 25.8 |
| Hemoglobin (g/dl) | 12.1 | pO2 (mmHg) | 71.4 |
| Platelets (×109/l) | 188 | BE (mmol/l) | -5.6 |
| C-Proteine Reactive (mg/dl) | >7 | HCO3- (mmol/l) | 17 |
| Creatinine (mg/dl) | 1.3 | Lactate (mmol/l) | 1.10 |
| PT-ratio (INR) | 1.26 | Sodium (mmol/l) | 145.8 |
| PTT-ratio | 1.10 | Potassium (mmol/l) | 3.29 |
Plain abdomen radiography was performed at the ED and showed distended stomach and small bowel with air-fluid levels (Fig. 1). No free gas in the peritoneal cavity was seen. A contrast-enhanced CT scan revealed a huge gastrectasia with liquids, small bowel distention due to a suspected adherent bridle. Some loops of the ileum showed emphysematous walls (Fig. 2). A minimal perihepatic liquid effusion was observed due to suffering bowel.

Plain abdomen radiography shows distended stomach and dilatated loops of bowel without free gas in the peritoneal cavity.
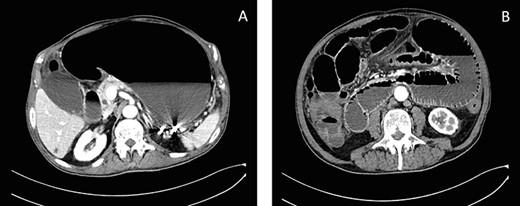
Axial CT scans of abdomen show gastrectasia with the NG tube just inserted (A) and a suspected image of bowel emphysematous walls (B).
A conservative approach was performed with antibiotic therapy, nasogastric (NG) and rectal tube insertion. Immediately 2000 ml of enterobiliary fluid came out from the NG tube and the symptoms improved. During the night, the patient removed the NG unintentionally, when a few hours later the tube was inserted again and 450 ml of fecal fluid were aspirated. The clinical signs and the worsened laboratory tests were highly suspicious for bowel obstruction and emergency surgery was indicated.
A supra-umbilical Hasson’s port was inserted and exploratory laparoscopy showed turbid effusion in Morrison’s pouch, spleno-renal pouch and pouch of Douglas. Two more trocars of 10 mm were inserted. Running the small bowel, a loop appeared densely adherent to the bladder and releasing the bowel from adhesions a bladder hole was found out (Fig. 3). The rupture of a bladder diverticulum was tamponade by an ileal loop and was critically inflaming the peritoneal cavity. An accurate laparoscopic adhesiolysis was performed. The ileal loops appeared vital and no bowel resection was necessary. The bladder hole was sutured with a knotless barbed suture. Dilute methylene blue was injected into the urinary catheter to check the watertight closure. No blue spreading was seen and a drain was inserted into pelvis. The surgery was performed by a skilled general surgeon and the consultant urologist wasn’t necessary.
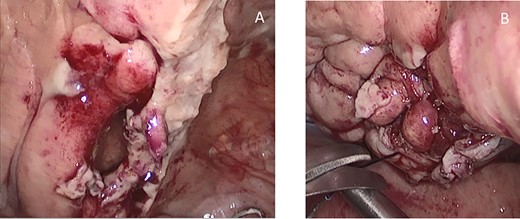
Intraoperative findings of the bladder diverticulum, before (A) and after (B) suture.
The postoperative course was characterized by Enterobacter aerogenes and Pseudomonas aeruginosa positive urine culture results. The drain was removed on the fifth postoperative day and the patient was discharged on the 14th postoperative day in good general conditions with the indwelling bladder catheter. The patient went to a rehabilitation center for 3 months and then he returned to his residential home for elderly. The follow-up was only by phone. He had an episode of urinary tract infection 4 months later due to the indwelling catheter. The Klebsiella pneumoniae urinary infection was treated with antibiotics without sequelae. Considering his conditions without symptoms, a postoperative cystography wasn’t performed.
DISCUSSION
Spontaneous bladder perforation is a rare event and represents a challenging diagnosis even with the aid of CT imaging. The risks of the rapture may be attributed to chronic inflammation such as infections or irradiation, to urinary retention due to outflow obstruction or neurogenic bladder, and to malignancies [1, 2]. Patients present acute abdominal pain and abdominal distension due to free fluid in peritoneal space. Most of the time, the diagnosis is intraoperatively as in our case. The misdiagnosis or delayed diagnosis of spontaneous bladder perforation can be life-threatening [5, 6]. Traumatic bladder ruptures are more common extraperitoneal and strictly connected with pelvic fractures, whereas the most frequent site of spontaneous ruptures is intraperitoneal. The guidelines of bladder perforation management suggest a conservative approach with the insertion of bladder catheter for extraperitoneal ruptures and surgery for intraperitoneal ones [7]. Exploratory laparoscopy can be safely performed also in emergency surgery and may offer a safe procedure with a high rate of correct identification in acute disease in many abdominal emergencies [8, 9]. Laparoscopy improves postoperative outcomes reducing the number of non-therapeutic laparotomies and days of recovery. CT cystography is recommended for a correct evaluation of each case when rupture is suspected [3]. In our case, the suspected preoperatively diagnosis was a bowel obstruction and exploratory laparoscopy turned out to be the therapeutic solution [4, 6, 10]. In the present patient, the tight phimosis with urinary retention and the indwelling catheter could be the greatest risk factors. We would like to emphasize that the presence of a urinary catheter does not preclude ruptures [2] and can hide urinary symptoms. Moreover, in our patient, we suspect that the bladder perforation probably occurred long before the gastro-intestinal symptoms.
CONCLUSION
In conclusion, emergency laparoscopic exploration is useful for the diagnosis and the treatment of spontaneous rupture of bladder diverticula. Urinary catheterization can be a risk factor of intraperitoneal bladder rupture. We hope that this case report can be useful to give these patients better outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
INFORMED CONSENT
Informed consent was obtained for all the patients enrolled in clinical research studies.
References
- computed tomography
- dilatation, pathologic
- intestinal obstruction
- intestine, small
- laboratory techniques and procedures
- laparoscopy
- sutures
- urinary retention
- urinary bladder
- diagnosis
- ileum
- phimosis
- bladder rupture
- urinary catheters
- abdominal pain, lower
- rebound tenderness
- emergency surgical procedure
- intraperitoneal rupture of bladder
- exploratory laparoscopy



