-
PDF
- Split View
-
Views
-
Cite
Cite
Takaya Suzuki, Taku Sato, Tohru Hasumi, Resection of a giant mediastinal atypical lipomatous tumor involving the esophagus, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa561, https://doi.org/10.1093/jscr/rjaa561
Close - Share Icon Share
Abstract
Liposarcoma is one of the common soft tissue tumors but barely arises from the mediastinum. Complete surgical resection with a negative surgical margin is required for the treatment; however, mediastinal liposarcomas tend to be large due to its slow-growing nature. A 57-year-old man was referred to us for having an abnormal mediastinal shadow in a chest X-ray. Computed tomography scanning revealed a giant posterior mediastinal tumor, completely involving the esophagus. Because of the unusual size and location of the tumor, we took a bilateral video-assisted thoracoscopic approach. First, the soft lipomatous compartment of the tumor was dissected from the esophagus and the descending aorta via the left thoracic cavity complete thoracoscopic procedure. Then, the patient was placed in the left lateral position, and the solid part of the tumor was completely resected using 13 cm of right-side thoracotomy. There was no complication or local recurrence in the first 26 months of follow-up.
INTRODUCTION
Soft tissue tumors of the mediastinum are rare, accounting for 2–6% of mediastinal malignancies [1]. Liposarcoma is the most common soft tissue tumor and can arise from a wide range of sites [2]. The retroperitoneum and lower extremities are common sites; however, liposarcomas are occasionally seen in the mediastinum [1]. Atypical lipomatous tumor (ALT), also called well-differentiated liposarcoma, is one of the histological categories of liposarcoma [2]. Due to their slow-growing nature, ALTs in the mediastinum cause only minimal symptoms and tend to be large when clinically detected. Surgery is commonly performed for mediastinal ALTs; however, the location and size often make surgery challenging. In this case, we successfully resection a giant posterior mediastinal ALT involving the esophagus under bilateral video-assisted thoracoscopic surgery.
CASE REPORT
A 57-year-old man was referred to our hospital due to an abnormal chest X-ray. His previous history included hypertension and subcortical intracerebral hemorrhage that was conservatively followed up without surgery. Chest X-ray demonstrated an enlarged mediastinum without loss of cardiac and diaphragmatic outlines (Fig. 1a). Computed tomography revealed a giant posterior mediastinal tumor composed of a well-circumscribed solid compartment with small calcifications, encapsulated by a fat-density compartment (Fig. 1b). The tumor extended longitudinally from the aortopulmonary window to the level of the diaphragm (Fig. 1b and c). The heart was deviated anteriorly by the tumor; however, the patient had no cardiac symptoms. The esophagus was completely involved in the fat-density compartment (Fig. 1b). Magnetic resonance imaging also indicated that the solid mass was surrounded by a fatty compartment (Fig. 1d–f).
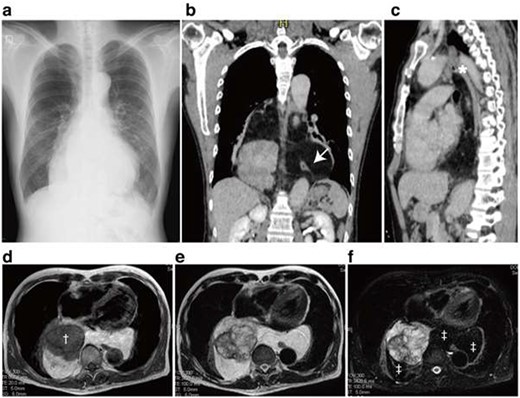
Chest X-ray, computed tomography and magnetic resonance imaging. A Chest X-ray demonstrated enlarged mediastinal shadow (a). Axial section revealed a posterior mediastinal tumor displacing the heart anteriorly (b). The well-capsulated tumor expanded into both thoracic cavities and involved the esophagus (b, Arrow). The superior border of the tumor reached the aortopulmonary window (c, asterisk). Magnetic resonance imaging of the tumor revealed the heterogeneous components in the tumor where a T1-low intensity component (†) was surrounded by fat components (‡) (d–f). T1-weighted image (d), T2-weighted image (e) and Fat-suppressed T2-weighted image.
Surgical resection was indicated, but we needed to decide the approach to the tumor carefully. Because the tumor was situated right behind the heart, it seemed difficult to remove the tumor via an anterior approach such as median sternotomy. Also, the tumor extended horizontally to bilateral thoracic cavities with close association to the vital anatomical structures such as the aortic arch, the pulmonary artery, the esophagus and the descending aorta (Fig. 1); therefore, en-bloc resection either by unilateral thoracotomy seemed to be unsafe. Consequently, we chose a bilateral approach in order to mobilize the tumor from the esophagus in left thoracoscopic surgery and then to completely remove the tumor using left thoracotomy. First, the patient was placed in the right lateral position. Four 5-mm access ports were created, and the subsequent procedures were performed under complete thoracoscopic technique with CO2. The soft lipomatous component of the tumor was bluntly and sharply dissected from the descending aorta and esophagus using laparoscopic dissectors and LigaSure™ laparoscopic sealer (Fig. 2b). After complete mobilization of the tumor (Fig. 2c), a chest drainage tube was inserted into the left thoracic cavity, and the left side procedure was finished. The patient was then placed in the left lateral position, and right posterolateral thoracotomy was performed using a 13-cm skin incision with muscle-sparing plus one 5-mm access port. The tumor was well encapsulated (Fig. 2d). The border of the tumor was easily determined because the most part of the posterior border of the tumor was mobilized by the left VATS. The anterior border of the tumor was bluntly dissected from the inferior vena cava (Fig. 2e), the inferior pulmonary vein and the pericardium (Fig. 2e). During the dissection procedure, we occasionally observed systemic hypotension by contracting the heart anteriorly. The tumor was then successfully resected en-bloc. Operation duration was 7 h and 12 min, with 960 g of bleed loss. The patient was discharged uneventfully on postoperative day 10.
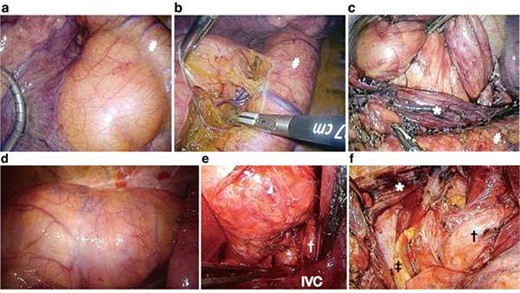
Operative findings. Operative findings in the left thoracic cavity (a–c). The tumor was situated between the aortopulmonary window (a) and diaphragm. The tumor was completely mobilized from the descending aorta (b) and esophagus with a complete thoracoscopic procedure (c). Operative findings in the right thoracic cavity (d–f). Most of the solid part of the tumor was situated in the right thoracic cavity (d). The tumor was dissected from important anatomical structures such as the inferior vena cava (e). The tumor was resected en-bloc via right thoracotomy (f). #Aorta, *Esophagus, †Inferior pulmonary vein, ‡Left lung, IVC; inferior vena cava.
The tumor weighed 1233 g and measured 22 × 15 × 9 cm (Fig. 3a). Pathological examination demonstrated scattered atypical mesenchymal cells with enlarged hyperchromatic nuclei consistent with the diagnosis of the ALT (Fig. 3b and c). There was no complication including swallowing problem or local recurrence in 26 months of follow-up.
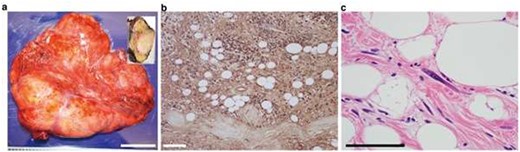
Pathological findings of the tumor. Macroscopic appearance of the resected tumor (a). The tumor cells were homogeneously S100-positive (b). Hematoxylin and eosin staining showed atypical spindle-shaped cells in the tumor (c).
DISCUSSION
Liposarcoma is the most common soft tissue tumor and typically arises in the lower extremities or retroperitoneum [3]. The World Health Organization histopathologic classification includes four distinct types of liposarcomas: ALT, dedifferentiated liposarcoma, myxoid cell liposarcoma and pleomorphic liposarcoma [2]. It is extremely rare, but all four types can arise from the mediastinum [1]. ALTs are considered to have a good prognosis, and surgical resection with a negative margin is important for the management of ALTs [4]. One of the difficult procedures, in this case, was how to separate the tumor from the esophagus, which was entirely engulfed by the tumor. Considering the relatively good prognosis of ATLs, it was unrealistic to remove the tumor with the esophagus. Therefore, we performed blunt dissection of the tumor followed by tumor splitting in order to completely separate the esophagus from the tumor. This procedure resulted in the exposure of the cut surface of the tumor; however, the process was sufficient for the en-bloc resection of the tumor in a significantly less invasive manner.
Mediastinal liposarcoma can be huge when detected due to its slow-growing nature [3]. Previous reports have described successful resection of large mediastinal liposarcomas, where several surgical approaches have been described [5–7]. In the majority of previously reported cases in which tumors were situated in the anterior mediastinum, an anterior approach such as median sternotomy or clamshell thoracotomy was employed [5, 7]. For the resection of middle/posterior mediastinal liposarcomas, unilateral thoracotomy was often adequate for full exposure of the tumor [8]. Because of the unique location and extent of the ALT in the current case; however, we thought that a median sternotomy or a posterolateral approach would not be useful for complete resection. Particularly in the present case, right thoracotomy seemed to be relatively unsafe for en-bloc tumor mobilization at the aortopulmonary window. The bilateral thoracoscopic procedure was able to provide excellent operative views in both thoracic cavities and enabled us to safely and gently mobilize the tumor from important organs such as the esophagus and the aorta. To our best of knowledge, this approach has not been used in previous reports [7]. This approach is potentially applicable to the cases in which tumors are situated in the posterior mediastinum.
AVAILABILITY OF DATA AND MATERIALS
All available data are included in this manuscript.
FUNDING
The authors have no funding source for this manuscript.
CONFLICT OF INTEREST STATEMENT
The authors have no financial or non-financial competing interests.



