-
PDF
- Split View
-
Views
-
Cite
Cite
J Bryan, J Ashcroft, V E Hudson, K Y Wong, Unusual presentation of appendicitis as soft tissue infection of the thigh, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa505, https://doi.org/10.1093/jscr/rjaa505
Close - Share Icon Share
Abstract
Appendicitis remains one of the most common causes of abdominal pain across the world typically presenting with right iliac fossa pain, fever and nausea or vomiting. We describe an unusual case of appendicitis presenting as a soft tissue infection of the thigh, thereby causing a delayed diagnosis from presentation. We discuss the pathophysiological process behind soft tissue infections caused by appendicitis and highlight investigation and management strategies to ensure prompt treatment to reduce patient mortality.
INTRODUCTION
Appendicitis remains one of the most common causes of abdominal pain across the world typically presenting with right iliac fossa pain, fever and nausea or vomiting. Timely management of appendicitis is crucial to prevent potential sequelae such as perforation, peritonitis and death.
CASE HISTORY
A normally fit and well 33-year-old woman presented to the emergency department with right flank and thigh pain for 3 weeks. She had previously been seen in primary care following 1 week of thigh pain, which was initially attributed to a musculoskeletal cause for which she was advised to take simple analgesia. The patient returned to the emergency department when the pain significantly worsened, and she developed an associated fever. Apart from a high body mass index, she had no other co-morbidities. On examination, she had diffuse erythema and tenderness over her proximal thigh, particularly marked on the medial aspect (Fig. 1). The erythema extended to her ipsilateral iliac crest. There was no palpable fluctuance or crepitus. Pain was exacerbated by movement at the hip joint, but there was no reduction in the range of movement. There was no guarding or tenderness on abdominal examination. At this time, her temperature was 39.3°C. She was tachycardic at 152 beats per minute but was normotensive, with a blood pressure of 111/57 mmHg. Her respiratory rate was 19, and she was saturating at 96% on air. Her white cell count was 19.2 (109/l), and her C-reactive protein was 148 (mg/l). She was scheduled for immediate surgical exploration of the flank and thigh under the plastic surgery team as necrotizing fasciitis could not be excluded. Given the atypical presentation, a prompt computed tomography (CT) scan of the abdomen and pelvis prior to surgical exploration was undertaken. This demonstrated large volume subcutaneous emphysema in the soft tissues of the thigh and flank. This was associated with a fistula tracking superior to the right iliac wing, originating from an appendiceal collection involving the iliacus muscle and the pelvic sidewall (Figs 2 and 3).

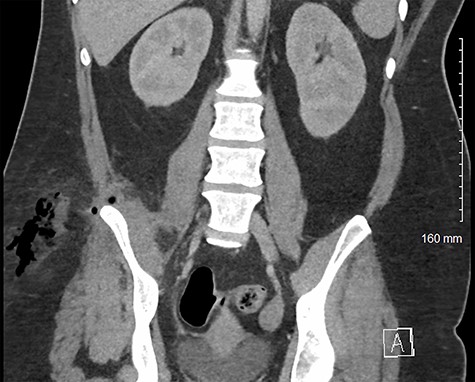
Coronal CT image of patient’s pelvis/abdomen demonstrating fistula tract containing gas and fluid from the intra-abdominal space through the inferior lumbar triangle into the soft tissue of the flank/proximal thigh.

Axial CT image of patient at L5 level, demonstrating inflamed perforated appendix adherent to the pelvic sidewall. This also shows an abscess in the subcutaneous fat of the flank/proximal thigh.
After discussion with the general surgical team, it was decided to proceed with surgical exploration of the thigh with conservative management of appendicitis. An abscess cavity in the deep fat associated with necrotic adipose tissue overlying the ilium was opened, debrided and washed out. There was no evidence of necrotizing fasciitis intraoperatively. Her appendicitis was managed medically with broad-spectrum antibiotics as it was felt that the adherent appendix would be too difficult to resect safely. A vacuum-assisted closure (VAC) dressing was used on the surgical site in the thigh. Microbiology swabs taken from the abscess cavity grew Streptococcus anginosus and Candida albicans. She was treated with co-amoxiclav, metronidazole and fluconazole. The patient recovered well post-operatively and did not require any organ support, despite persistent fevers. She returned to theatre twice weekly for wound washout and VAC dressing change. Cultures from the subsequent washout fluid grew Escherichia coli, which was identified as an extended-spectrum beta-lactamase-producing organism. The antibimicrobial regimen was changed to meropenem and fluconazole, after which her pyrexia resolved.
During her admission, she had a repeat CT scan that demonstrated features of chronic inflammation of the terminal ileum, as well as additional inflammation island more proximally in the ileum. Biopsies taken from the large bowel showed preserved crypt architecture and no specific features of inflammatory bowel disease. Biopsies of the caecum showed mild chronic inflammation that was felt to be in keeping with perforated appendicitis. She was discharged to outpatient care after 6 weeks with a low-volume enterocutaneous fistula, managed with simple dressings.
DISCUSSION
Appendicitis typically presents with abdominal pain that starts centrally and then shifts to the right iliac fossa as peritonitis develops; a retrocaecal appendix is a recognized risk factor for occult and unusual presentation [1]. This case occurred in the COVID-19 pandemic. It is recognized that the rate of hospital presentations was lower in this period due to fear of contracting the virus, and this may have been a contributing factor to the delayed presentation of this patient [2]. Unusual presentations of appendicitis are well described in the literature. For example, appendicitis can present as soft tissue infection of the abdominal wall, flank, thigh and perineum, the most serious complication of which being necrotizing fasciitis [3]. Most of the similar presentations to our case describe retroperitoneal spread of infection, tracking down the fascial plane of the psoas muscle into the thigh [4–6]. In our case, the infection fistulated through the posterior abdominal wall.
There are two areas of relative weakness in the posterior abdominal wall; these are the superior and inferior lumbar triangles. The inferior lumbar or Petit’s triangle is bordered by the iliac crest inferiorly, the external oblique laterally and the latissimus dorsimedially. The floor is formed by the internal oblique muscle. This triangle is the route of extra-abdominal egress of infection in this case. Retroperitoneal abscess tracking through the inferior lumbar triangle of Petit, similar to this case, is also cited by other reported cases [7, 8]. As far as we could find, there are no documented cases of infection spreading through the superior lumbar triangle.
In this case, prompt surgical exploration prevented development of sequelae such as necrotizing fasciitis. The patient’s complex appendicitis was successfully managed medically alongside surgical management of the associated abscess. Atypical soft tissue infections, particularly around the abdomen and thighs, should be investigated with imaging preoperatively, if this can be performed in a timely manner. The use of CT imaging played an important preoperative diagnostic role in this case in identifying the source of infection.
CONFLICT OF INTEREST STATEMENT
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organization that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
CONTRIBUTORSHIP STATEMENT
J.B, J.A. and K.Y.W. undertook conceptualization of this article. J.B, J.A. and V.H. drafted and revised the manuscript. K.Y.W. undertook critical review of the manuscript and guided critical revisions. K.Y.W. approved final manuscript for submission.
TRANSPARENCY DECLARATION
J.B. as lead author affirms that the manuscript is an honest, accurate and transparent account of the case being reported and that no important aspects of the case have been omitted.



