-
PDF
- Split View
-
Views
-
Cite
Cite
Matthew G K Benesch, Angela S D Bussey, Necrotizing fasciitis from perforated sigmoid diverticulitis with subsequent pyoderma gangrenosum: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa282, https://doi.org/10.1093/jscr/rjaa282
Close - Share Icon Share
Abstract
Postsurgical pyoderma gangrenosum is a very rare form of cutaneous ulceration that is poorly recognized outside of dermatology and in some circumstances has been mistaken for necrotizing fasciitis. Here, we present a rare case of sigmoid diverticulitis with left ureter obstruction that perforated and quickly progressed into necrotizing fasciitis of the left buttock and leg via retroperitoneal spread in an immunocompetent patient. Nearly a year after intense surgical therapy, the patient rapidly developed ulcerating lesions over the left hip which presented a diagnostic dilemma. These were initially thought to represent Marjolin’s ulcers, which would require aggressive local excision. Multiple diagnostic imaging tests and biopsies eventually confirmed pyoderma gangrenosum, which was successfully treated with immunosuppressive therapy. This case highlights the need for a very broad differential diagnosis and wide expertise consultation when managing unusual postsurgical complications, especially when treatment modality critically depends on the correct diagnosis.
INTRODUCTION
Colonic diverticulitis is a common manifestation in up to 25% of patients with diverticulosis, with most occurring in the sigmoid colon [1]. Extraperitoneal findings from diverticular disease occur in less than 2% of cases, and necrotizing fasciitis (NF) is even rarer (<1%) [2]. NF is an aggressive polymicrobial infection of subcutaneous tissues which rapidly spreads through fascial planes [3]. The estimated incidence is four cases per 1 million with a mortality rate of about one-third [2, 3]. Primary treatment involves radical debridement of infected tissue. Risk factors include advanced age, peripheral vascular disease, diabetes mellitus, immunosuppression, obesity and malnutrition [4].
Pyoderma gangrenosum (PG) is a rare neutrophilic dermatosis characterized by aseptic neutrophilic inflammation [5, 6]. There are several variants including ulcerative, bullous, pustular, vegetative, peristomal and postsurgical [5]. It is most commonly seen in patients with an underlying immunological disorder such as inflammatory bowel disease [5].
In this report, we present a patient with NF of the left buttock and leg secondary to perforated sigmoid diverticulitis. Despite having minimal medical comorbidities and no known immunological disorder, she later developed postsurgical PG several months after initial presentation.
CASE REPORT
A 61-year-old female presented to emergency with a rapidly worsening soft tissue infection of her left buttock extending to her posterior thigh. Her recent medical history was unusual. Previously healthy and taking no regular medications, she developed a chronic left perineum sinus which was excised 2 years prior to presentation. A CT scan and colonoscopy as part of her workup uncovered asymptomatic sigmoid diverticulosis. A year later she developed a left maxillary sinus mass with a radiographical differential diagnosis including granulomatosis with polyangiitis (final pathology on excision showed only osteomyelitis). Repeat CT scan during this workup now showed new left-sided hydronephrosis overlain with inflammatory changes in keeping with a chronic sigmoid diverticulitis (Fig. 1), despite an otherwise clinically asymptomatic abdomen. Colorectal carcinoma was ruled out by a repeat colonoscopy 8 months prior to presentation. The hydronephrosis was managed by ureteric stenting, and the patient opted for conservative management of her diverticulitis.
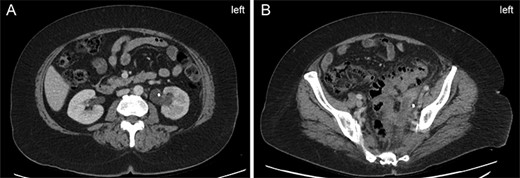
Left-sided hydronephrosis 6 months prior to presentation. (A) Left-sided hydronephrosis demonstrated at renal hilum with ureteric stent in place. (B) Demonstration of extensive diverticuli and surrounding inflammatory changes in the same CT scan as Panel A. Uretic stent is again seen.
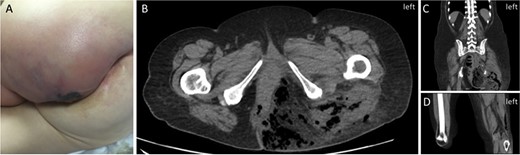
Initial patient presentation. (A) Initial presentation of left buttock on physical exam. (B) CT scan (axial view) demonstrating free air in left buttock. (C) CT scan (coronal view) demonstrating free air in the left thigh. (D) CT scan (coronal view) demonstrating free air extending into left popliteal fossa.
Four weeks prior to presentation, she developed a blistering rash over her left buttock and gluteal fold that did not cross midline. She was treated for 10 days with acyclovir for shingles with good response. Three days prior to presentation, she visited the emergency room again with a new painful induration over her left buttock that was diagnosed as an early abscess and prescribed amoxicillin–clavulanate.
At presentation, this induration had enlarged with a 1-day history of serous discharge and chills (Fig. 2A). All vital signs were normal, but bloodwork revealed leukocytosis of 22 200 and acute kidney injury with a creatinine of 191 μmol/L. Non-contrast CT scan showed performed sigmoid diverticulitis with free air tracking inferiorly into the left pelvis with a 5.5 × 3.3-cm abscess. Significant extension of gas was also seen throughout the entire left buttock tracked posteriorly along the hamstring muscles to the popliteal fossa (Fig. 2B–D). Subcutaneous emphysema rapidly became clinically apparent, and she was taken to the operating room for wide debridement of the left buttock, perineum and leg, with laparotomy, washout and left hemicolectomy (Fig. 3A). Antibiotic treatment with piperacillin/tazobactam, clindamycin and vancomycin was initiated. She was taken back to the operating room the next day for further debridement, drainage of retroperitoneal and pre-rectal abscesses, and end colostomy creation. Final tissue culture revealed polymicrobial gut flora. After 19 days in the intensive care unit, she was transferred to the floor and continued treatment with negative pressure wound therapy for an additional month prior to transfer to a rehabilitation hospital. She returned to the operating room 2 months after initial presentation for delayed wound closure with a rotational flap on the left buttock (Fig. 3B). The left ureteric stent was removed 1 week later, and resolution of hydronephrosis was confirmed on subsequent imaging. Six months after presentation, she developed ulcerating lesions over her left hip. These were biopsied on two separate occasions as the initial suspicion was they represented Marjolin’s ulcers, which are aggressive ulcerating squamous cell carcinomas in areas of previously traumatized, chronically inflamed and scarred tissue and are treated by wide local excision. Instead, they ultimately revealed PG (Fig. 3C), which is not a surgically treated condition. She was consulted to dermatology and initially treated with prednisone, colchicine and azathioprine. Now 2.5 years since presentation, she is chronically maintained with mycophenolic acid and intralesional triamcinolone injections with good effect. Multiple subsequent investigations for immunodeficiency syndromes have been negative.
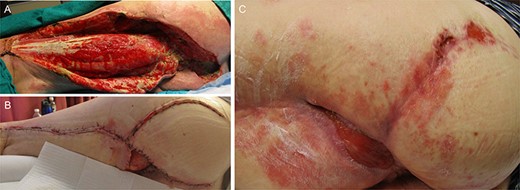
Photographs of the clinical course of the wound. (A) Left buttock and thigh 16 days after initial debridement. (B) Left buttock and thigh after delayed closure and rotational flap 2 months after initial surgery. (C) Development of pyoderma gangrenosum particularly noticeable over the left hip 6 months after surgery.
DISCUSSION
There are a handful of case reports describing NF involving the lower extremities originating from colonic diverticulitis [7, 8]. Most of these patients are immunosuppressed [3, 7, 8]. To our knowledge, this is the only reported case of PG in a patient previously treated for NF. Instead, there are several reports of PG misdiagnosed as NF and mistakenly treated with surgical debridement [9, 10]. Most postsurgical PG occur on the breast and trunk within 7 days of surgery, but cases of peristomal PG in patients with underling inflammatory bowel disease have an onset up to 48 months [5]. In our patient, clinical manifestations of PG were delayed by several months. Multiple biopsies at different times were taken prior to arrival at this diagnosis, as the initial clinical suspicion of Marjolin’s ulcers if acted upon would have led to inappropriate surgical excision. Given this patient’s unusual additional previous history of maxillary osteomyelitis, it is possible she may have an underlying immunological disorder not yet characterized. Patients with PG requiring subsequent surgery appear to benefit from perioperative steroids to prevent PG recurrence [5]. A primary learning point from this case is postoperative ulcerating lesions may need to be biopsied and cultured numerous times to arrive at a definitive diagnosis prior to initiating definitive treatment. Broad consultation is also recommended, as PG is uncommonly considered on the differential for surgical patients.
CONFLICT OF INTEREST STATEMENT
There are no potential conflicts of interest on the part of any named author.
Funding
None.
ACKNOWLEDGEMENTS
We wish to thank Margo Cashin for the provision of photographs.



