-
PDF
- Split View
-
Views
-
Cite
Cite
Afieharo I Michael, Olayinka A Olawoye, Odunayo M Oluwatosin, Concentric mastopexy for pubertal gynaecomastia in an African child, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa276, https://doi.org/10.1093/jscr/rjaa276
Close - Share Icon Share
Abstract
Gynaecomastia refers to the enlargement of the male breast. It can be psychologically disturbing for children and adolescents as well as adults. While in children watchful waiting is advised as the gynaecomastia could resolve, surgical intervention becomes necessary where there is significant psychosocial disturbance. We present a case of an African child whose quality of life improved after correcting the gynaecomastia. We highlight the concentric mastopexy method in the surgical management of gynaecomastia.
INTRODUCTION
Gynaecomastia refers to enlargement of the male breast. Its occurrence could be physiological or pathological [1]. Physiological gynaecomastia is seen in the neonatal period, puberty and old age. In these instances, there is an imbalance in the oestrogen/androgen ratio in favour of the former [1, 2]. Pathologic gynaecomastia occurs in disease conditions such as liver cirrhosis and testicular cancer. It has also been associated with use of certain drugs such as oral contraceptives, tricyclic antidepressants, cimetidine, etc. [2]. In children it could occur from as early as 8 years [3]. It is more commonly bilateral, though unilateral occurrences have been reported [3, 4]. The natural history of prepubertal and pubertal gynaecomastia is resolution after a few (1–3) years. Gynaecomastia is usually asymptomatic and reassurance of the parents and child is sufficient in most cases [5]. However, when there is associated persistence of pain or psychosocial embarrassment surgery is indicated [3, 4].
Simon classified gynaecomastia into three main categories based on the clinical features of the enlarged breast [6]. This classification has been used to determine the method of surgical intervention required [7]. Subcutaneous mastectomy, liposuction and open excision with skin reduction are methods employed in the surgical management of gynaecomastia [1, 3, 7]. We report this case in which we performed subcutaneous mastectomy using the concentric mastopexy technique in the correction of pubertal gynaecomastia.
CASE REPORT
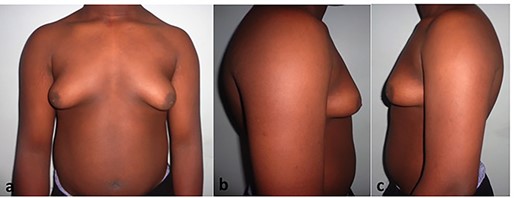
An 11-year-old boy presented to us with his parents on account of bilateral breast enlargement (Fig. 1a–c). This had been on for 2 years prior to presentation. There was no associated pain in the breasts; he was not on any medication and he had no intercurrent medical illness. The size of his breasts had severely affected his quality of life. He insisted on wearing at least four layers of clothing before he left his home for any outing. He had stopped swimming, a sport he liked very well and was very wary of going into the boarding school.

Preoperative markings (a), intraoperative excision of breast tissue (a), post-operative compression dressing (a).
On examination, he was a healthy looking with a body mass index of 20. The only clinical signs were the moderately enlarged breasts with some skin redundancy bilaterally. The nipple–areolar complexes were above the inframmamary folds. Definite breast glandular tissue could be palpated beneath the skin bilaterally. A diagnosis of Simon’s Grade IIb gynaecomastia was made. He was scheduled for a subcutaneous mastectomy after appropriate counselling. Neither he nor the parents were willing to wait anymore to determine if it would resolve spontaneously.
OPERATIVE TECHNIQUE
Preoperative markings, as illustrated in Figure 2a, were done for concentric mastopexy using the second rule as described by Spear et al. [8]. A third-generation cephalosporin was given at induction of anaesthesia. Under general anaesthesia and with the patient in the supine position, the operating field was prepared and draped. Both breasts were infiltrated with 200 ml of tumescent fluid. The concentric skin around the areolar was de-epithelialized. A semilunar incision was then made from nine to three o’clock positions at the junction of the areolar and the de-epithelialized area. This was deepened through the subcutaneous plane to the breast tissue. The breast tissue was grasped with an Allis forceps and a McIndoe’s scissors used to separate the breast tissue from the overlying subcutaneous tissue and the underlying pre-pectoral fascia. Care was taken to maintain 1.5 cm of subcutaneous tissue beneath the nipple areolar complex (NAC) to avoid a post-operative depression of the NAC. The breast tissues were excised en masse (Fig. 2b) and sent for histological examination. The resultant cavities were irrigated and vacuum drains inserted. The wounds were closed with 4/0 monocryl deep dermal stiches. First, at 12, 6, 3 and 9 o’clock positions and subsequently bisecting the residual defects. Skin approximation was done using 5/0 monocryl as subcuticular stitches. The drains were removed on the third post-operative day. He was discharged on compression garment (Fig. 2c) for 4 weeks. At the one-year follow-up he came with only one shirt on, there was very satisfactory breast shape with minimal scarring (Fig. 3a–c). He had also returned to swimming.
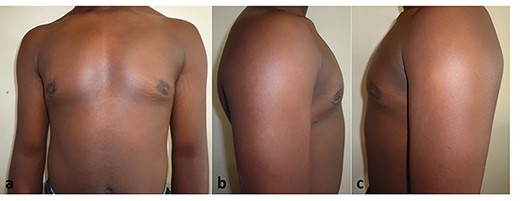
a–c. One-year post-concentric mastopexy for pubertal gynaecomastia.
DISCUSSION
The psychosocial improvement in our patient was quite remarkable. We cannot say whether the gynaecomastia would have resolved if the decision had been taken to wait but this risk would have been at the expense of the psychological stability or quality of life of this child. Psychological disturbance is a well-documented reason for surgical intervention for gynaecomastia in children and adolescents [4, 5, 9]. Firriolo et al. [9] have espoused the improved quality of life following surgical treatment for gynaecomastia. They determined that within a year following surgery for gynaecomastia in adolescents, the health-related quality of life was similar to those of the controls.. The prior psychosocial deficits had been alleviated as was seen in our case.
Subcutaneous mastectomy through an intra-areolar approach is the traditional method for surgical treatment of gynaecomastia [10]. Subcutaneous mastectomy alone would, however, not take care of the excess skin as seen in Simon’s Grade IIb and III gynaecomastia [1, 6]. We harnessed the advantage of the concentric mastopexy technique as described by Spear et al. [8] to excise the redundant skin in this case. This method places the scar on the areolar margin, which could be inconspicuous as seen in this patient. Although widening of the areolar is a possible complication of this technique, we did not encounter it in this case. The use of a purse string suture in the outer concentric circle can be used to forestall this complication [7]. Our patient may have benefitted from liposuction, which gives even less scarring; however, liposuction equipment was not available in our centre at the time. Complications of the subcutaneous mastectomy could be the formation of haematoma or seroma [7]. Although we used drains in our patient, some authors do not use drains [1, 2]. It is important to appropriately determine the Simon’s grade of the gynaecomastia prior to deciding on the best method of surgical intervention.
CONCLUSION
We have reported improved psychosocial functioning following concentric mastopexy for pubertal gynaecomastia in an African child.
Conflict of interest statement
None declared.



