-
PDF
- Split View
-
Views
-
Cite
Cite
Lauren E Smith, and Paul Levy, Ischemic appendicitis due to pelvic adhesions: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa055, https://doi.org/10.1093/jscr/rjaa055
Close - Share Icon Share
Abstract
Acute appendicitis is one of the most common etiologies of a surgical abdomen. The lifetime risk is estimated to be 7%. Over 300 000 appendectomies occur annually in the USA. The pathophysiology of appendicitis in most patients is believed to be caused by outflow obstruction of the appendiceal lumen leading to increased intraluminal pressure, venous congestion and mucosal ischemia. This can occur due to a variety of internal obstructive causes such as a fecalith, lymphoid hyperplasia, parasites or a tumor. To date, no case reports describing appendicitis secondary to external compression of the appendix leading to outflow obstruction been documented in the literature. This case report describes a 61-year-old female who had a thick, adhesive band compressing the base of her appendix, which created external outflow obstruction leading to the development of appendicitis.
INTRODUCTION
Acute appendicitis is one of the most common etiologies of a surgical abdomen. The lifetime risk is estimated to be 7%. Over 300 000 appendectomies occur annually in the USA [1,2]. The first known case of appendicitis was documented by Claudis Amyand in 1735. Since his account, the pathophysiology and management of appendicitis have evolved drastically [3]. To date, no case reports describing appendicitis secondary to external compression of the appendix leading to outflow obstruction been documented in the literature. This case report describes a 61-year-old female who had a thick, adhesive band compressing the base of her appendix, which created external outflow obstruction leading to the development of appendicitis.
CASE REPORT
A 61-year-old female presented to the emergency room complaining of sharp lower right abdominal pain of 2 days duration; she also admitted to chronic intermittent abdominal pain over the past 2 months. She denied any fever, chills, nausea, vomiting, chest pain or shortness of breath. She did admit to cyclical episodes of diarrhea and constipation. Her past medical history was significant for antiphospholipid antibody with recent stroke and venous sinus thrombosis, lupus and hypothyroidism. Her past surgical history included: caesarian section, total abdominal hysterectomy, laparoscopic cholecystectomy and a total knee replacement. Her family history was negative for any types of inflammatory bowel disorder. Socially, she was married and denied any history of smoking, drug or alcohol use. She took the following medications daily: Coumadin 15 mg, Plaquenil 200 mg and Levothyroxine 25 mcg.
On physical exam, she was noted to be afebrile and normotensive. The abdomen was soft with tenderness to palpation in the right lower quadrant. There were normoactive bowel sounds. Laboratory data demonstrated a white blood count of 5300, a hemoglobin of 14.4 and a hematocrit of 43%. Renal function, electrolytes, liver function and urinalysis were all within normal ranges. Her international normalized ratio was 3.5.
A CT of the abdomen and pelvis without contrast was obtained on admission and revealed a dilated appendix up to 1.5 cm in size with no evidence of obvious appendicolith (Fig. 1). There was evidence of extensive mesenteric edema in the right lower quadrant of the abdomen. It was felt that these findings were consistent with appendicitis with possible early rupture pattern. Due to her history and likely early ruptured appendicitis, she was felt to be a high surgical risk and she was initially treated on the interval appendicitis pathway. This included IV antibiotic therapy and a repeat CT scan of the abdomen/pelvis 48 h after initial presentation. She was also placed on a heparin drip and her Coumadin and Plaquenil was held.

Axial slice of the CT of the abdomen/pelvis demonstrating a dilated appendix up to 1.5 cm in size with mesenteric edema in the right lower quadrant of the abdomen.
Forty-eight hours after admission, the patient remained afebrile and her vital signs were stable within a normal range. Her laboratory data were as follows: white blood cell count 2500, a hemoglobin of 12, a hematocrit of 35.3%, and her renal function, electrolytes, and liver function remained within normal ranges. She continued to complain of worsening right lower quadrant abdominal pain. A repeat CT scan of the abdomen/pelvis with IV and oral contrast demonstrated a persistent dilated appendix up to 1.5 cm with surrounding inflammatory changes. There was no evidence of any loculated fluid collections or abscess identified.
There was concern that the patient was not mounting an appropriate response to infection due to her history of immunomodulator use. Therefore, it was decided to take the patient to the operating room for a diagnostic laparoscopy with likely appendectomy. Once in the abdomen, an edematous and ischemic-appearing appendix was visualized in the right lower quadrant. There was a thick adhesive band noted to be compressing the base of the appendix (Fig. 2). This band was connected to scar tissue along the left ovary and fallopian tube. An ultrasonic energy device was used to take down the adhesive band in its entirety. An appendectomy was also performed.
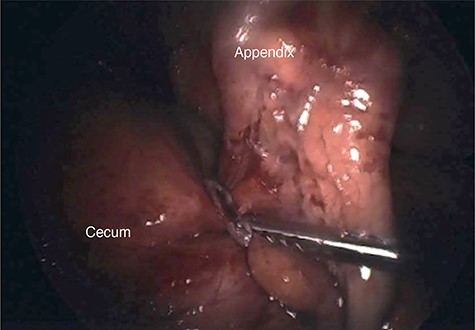
Intraoperative photograph of a thick adhesive band noted to be compressing the base of the appendix.
The appendix was sent to pathology for further evaluation. The pathological analysis revealed ischemic changes with fibroplasia and hemorrhage of the serosal surfaces. There was no evidence of any neutrophilic invasion to indicate an infective process. There were no malignant features identified.
The patient did well post-operatively and she was discharged home 2 days after surgery. The patient was seen at 2-week follow-up. She reported complete resolution of her previous symptoms. She was instructed to follow-up on an as-needed basis.
DISCUSSION
In 1886, Reginald Fitz became one of the first physicians to propose a theory regarding the pathophysiology of acute appendicitis. The most widely accepted pathophysiology of appendicitis in most patients is due to outflow obstruction of the appendiceal lumen. The lack of a patent appendiceal lumen creates increased intraluminal pressure, bacterial overgrowth, and venous congestion thus leading to mucosal ischemia. This can occur due to a variety of internal obstructive causes such as a fecalith, lymphoid hyperplasia, parasites or a tumor [2,3]. As medicine continues to progress, more obscure and unusual etiologies of acute appendicitis are being discovered [2–5]. External obstructive causes of acute appendicitis have not been well documented in the literature. To the authors’ knowledge, this report is one of the first that describes external obstruction from an adhesive band as the cause of the patient’s acute appendicitis.
The management of acute appendicitis has become controversial. Appendicitis has largely been considered a surgical condition; however, more conservative non-operative approaches have recently been employed [1, 3, 5]. Meta-analyses of these studies have suggested that non-operative management of acute appendicitis tends to be inferior; however, higher quality studies are needed. As a result, appendectomy is still considered to be the gold standard for uncomplicated appendicitis. Initial non-operative treatment of appendicitis with perforation and abscess formation is the preferred choice with the establishment of adequate source control.
The option for an interval appendectomy is also debated [4–6]. Due to the particular etiology of our patient’s appendicitis, she would have likely failed a conservative non-operative pathway.
Ultimately, this case adds to the growing body of literature regarding diverse etiologies of acute appendicitis. These etiologies should be taken into consideration when determining a treatment pathway for a patient with appendicitis.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICAL APPROVAL
Ethical approval from the Kettering Health Network institutional review board was obtained (IRB #19-081).
CONSENT
Consent from the patient for this case report was obtained.
References



