-
PDF
- Split View
-
Views
-
Cite
Cite
Masato Furui, Jeswant Dillon, Kunwar Muhammad Aqeel Akhtar, Ahmad Nazrin Bin Ja’apar, Ruptured sinus of Valsalva aneurysm with ventricular septal defect complicated by preoperative cardiogenic shock, cardiac arrest, and multiple organ dysfunction: a rare survivor and review of contemporary literature, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa567, https://doi.org/10.1093/jscr/rjaa567
Close - Share Icon Share
Abstract
Sinus of Valsalva aneurysm (SVA) is a relatively rare cardiac condition, in which the patient is usually asymptomatic. However, once this aneurysm ruptures, patients present with acute symptoms of heart failure. Timely surgical intervention is essential.
We present the case of a 27-year-old woman, who had a ruptured SVA with a ventricular septal defect (VSD). The patient collapsed before the emergency operation and needed cardiopulmonary resuscitation. The patient required preoperative high inotoropic support and postoperative management was difficult because of multiple organ dysfunction. However, the patient recovered after using inhaled nitric oxide and veno-venous hemofiltration and tracheostomy, and was discharged with no further complications. To the best of our knowledge, no such case of a ruptured SVA with VSD, complicated by preoperative cardiac arrest and multiple organ dysfunction that culminated in a successful recovery, has been reported to date.
INTRODUCTION
Sinus of Valsalva aneurysm (SVA) is a rare cardiac condition, in which the patient is usually asymptomatic. The etiology of SVA is commonly a defect in the aortic media. SVA presents congenitally or following injury, endocarditis, Behcet’s disease, Marfan syndrome, Ehlers–Danlos syndrome or other connective tissue disorders [1, 2]. However, SVAs rupture observed in 34–40% of patients, and 17–25% of these patients experience acute symptoms of heart failure such as dyspnoea, fatigue and chest pain [1–3]. Urgent surgical intervention is required to improve patient outcomes, but these outcomes depend on the degree of intra-cardiac shunt, other cardiac anomalies, co-morbidities, age and preoperative status of the patient. This report presents a case of a ruptured SVA with ventricular septal defect (VSD) in a critical condition, yet achieved a successful outcome due to timely surgical intervention despite preoperative cardiac arrest and multiple organ dysfunction. In our case, cardiogenic shock and multiple organ dysfunction progressed rapidly following the rupture of the SVA.
CASE REPORT
A 27-year-old woman with underlying VSD presented to a local hospital with sudden onset of cough and pleuritic chest pain. The patient was intubated in the emergency department because of tachycardia, tachypnoea and severe dyspnoea. Her vital signs revealed a blood pressure of 98/78 mmHg and a heart rate of 130 bpm, and she was afebrile. Physical examination showed a continuous murmur on auscultation of the anterior chest wall.
An electrocardiogram showed sinus tachycardia and ST depression in leads V4-V6. A chest X-ray revealed severe lung congestion and cardiomegaly. Transthoracic echocardiography (TTE) showed a ruptured SVA connecting to the right ventricle (RV), a subarterial VSD measuring 10 × 12 mm, with a left ventricular ejection fraction of 47% and normal valve function with mild tricuspid regurgitation (Fig. 1). No clot or vegetation was observed. Blood tests revealed a white blood cell count of 31 000/L, serum creatinine of 321 μmol/L, aspartate aminotransferase of 5199 U/L and alanine aminotransferase of 3458 U/L. The patient was diagnosed with ruptured SVA with VSD in cardiogenic shock and transferred to our hospital for further management.
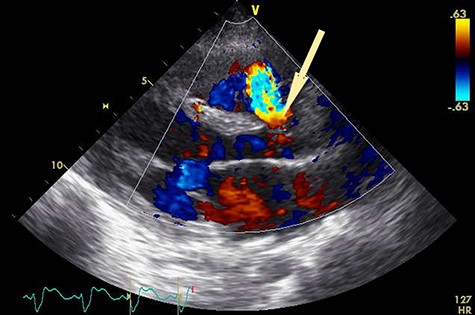
Preoperative transthoracic echocardiogram. Shunt flow (arrow) from aorta to RV.
An emergency operation was planned. However, just before the operation, the patient sustained a cardiac arrest secondary to cardiogenic shock. She was revived after 7 min of cardio-pulmonary resuscitation (CPR), supported with high doses of inotropes, i.e. intravenous noradrenaline at 0.3 μg/kg/min, adrenaline at 0.15 μg/kg/min, vasopressin at 3 unit/h, and dobutamine at 20 μg/kg/min. Because of the patient’s rapidly deteriorating condition, a multidisciplinary team conference was held, and a high-risk informed consent was obtained from the patient’s family for an emergency operation.
After sternotomy, cardiopulmonary bypass (CPB) was established with ascending aortic and bicaval cannulations, and systemic cooling lowered the body temperature to 32°C. The aorta was cross clamped, and an oblique aortotomy was performed. Antegrade cardioplegia was delivered into the coronary ostia with left ventricle venting via the right superior pulmonary vein. After arresting the heart, the ruptured SVA was identified by a thorough inspection (Fig. 2). There was no vegetation. The main pulmonary artery was opened with a vertical incision, and the VSD was found just below the aortic annulus.
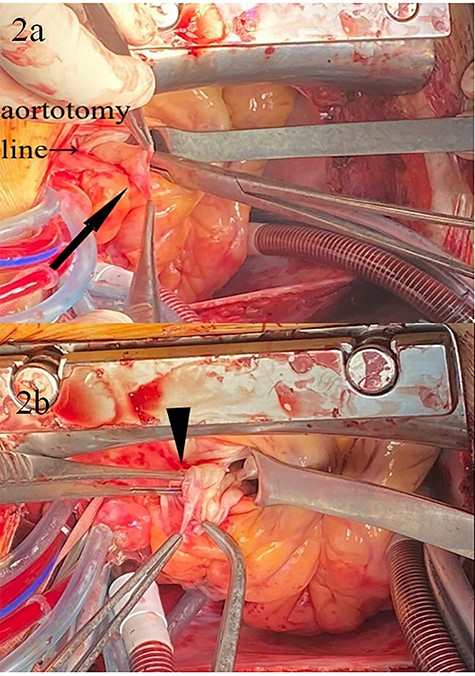
Intraoperative images; (a) SVA (arrow); (b) the rupture site (arrowhead) of SVA; forceps are inserted into the ruptured hole.
Subsequently, repair of the SVA and VSD closure were completed with two separate Gore-tex® 0.4 mm patches. The patient was rewarmed and weaned off CPB with high dose inotropic support. Postoperative transoesophageal echocardiogram showed no residual shunt or aortic regurgitation, and the patient was transferred to the intensive care unit. The aortic cross-clamp time, CPB time, and total operative times were 54, 119 and 293 min, respectively.
Postoperatively, the patient required prolonged intensive care. Inhaled nitric oxide for 3 days and continuous veno-venous hemofiltration for 10 days supported the patient and significantly improved blood parameters, which gradually normalized in the following days. A postoperative TTE revealed no shunt or aortic regurgitation (Fig. 3). However, a tracheostomy was performed on postoperative day (POD) 15 because of prolonged ventilation. The patient was discharged on POD 55 in a stable condition after de-cannulation of the tracheostomy tube.
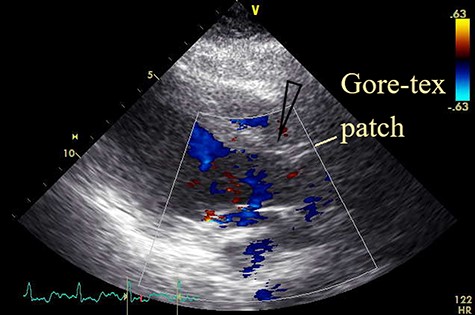
Postoperative transthoracic echocardiogram; the view after patch closure by Gore-tex® 0.4-mm patch with no shunt flow (open arrowhead).
DISCUSSION
Patients with ruptured SVA are likely to die within 1–3.9 years if left untreated, and the complication rate of congestive heart failure is approximately 10% [1–3]. In our case, the patient experienced cardiac arrest preoperatively as a result of worsening congestive heart failure and cardiogenic shock, which indicated that the patient was gravely ill. The Euro Score and Euro Score II for the patient were 12.0% and 42.6%, respectively, although it was a high risk we felt compelled to perform an emergency operation because of her age. Reviewing the literature, we found six cases of ruptured SVA, which experienced circulatory collapse or cardiac arrest, and all of them expired (Table 1) [4–8]. Our patient was unique, in that she underwent 7 min of CPR and had discoloration of peripheries due to hypo-perfusion and high doses of inotropes with multiple organ dysfunction at the time of operation and yet survived. As a result of timely intervention, postoperative haemodynamics and organ functions improved dramatically.
Reported cases and outcomes of ruptured SVA complicated by preoperative circulatory collapse or cardiac arrest
| Author . | Year published . | No of Pts . | Age . | Diagnosis . | Surgical intervention . | Cause of death . | Outcome . |
|---|---|---|---|---|---|---|---|
| Munk et al. | 1999 | 1 | 35 years | Ruptured SVA | – | Cardiac tamponade | Died preop |
| Doevendans et al. | 2001 | 1 | 67 years | Ruptured SVA | Repair of SVA | Cardiac tamponade | Died postop |
| Lee et al. | 2013 | 1 | 39 years | Ruptured SVA | Repair of SVA | AMI | Died postop |
| Liu et al. | 2014 | 1 | 17 years | Ruptured SVA | – | MOF | Died preop |
| Gilbert et al. | 2017 | 2 | 9 months | Pseudoaneurysm of SoV | – | Cardiac tamponade | Died preop |
| 13.5 months | Pseudoaneurysm of SoV | – | Arrhythmia possibly complicating sepsis | Died preop | |||
| Present case | 2020 | 1 | 27 years | Ruptured of SVA | Repair of SVA and VSD closure | – | Survived |
| Author . | Year published . | No of Pts . | Age . | Diagnosis . | Surgical intervention . | Cause of death . | Outcome . |
|---|---|---|---|---|---|---|---|
| Munk et al. | 1999 | 1 | 35 years | Ruptured SVA | – | Cardiac tamponade | Died preop |
| Doevendans et al. | 2001 | 1 | 67 years | Ruptured SVA | Repair of SVA | Cardiac tamponade | Died postop |
| Lee et al. | 2013 | 1 | 39 years | Ruptured SVA | Repair of SVA | AMI | Died postop |
| Liu et al. | 2014 | 1 | 17 years | Ruptured SVA | – | MOF | Died preop |
| Gilbert et al. | 2017 | 2 | 9 months | Pseudoaneurysm of SoV | – | Cardiac tamponade | Died preop |
| 13.5 months | Pseudoaneurysm of SoV | – | Arrhythmia possibly complicating sepsis | Died preop | |||
| Present case | 2020 | 1 | 27 years | Ruptured of SVA | Repair of SVA and VSD closure | – | Survived |
AMI, acute myocardial infarction; MOF, multiple organ failure; Postop, postoperative; Preop, preoperative; Pt, patient; SoV, sinus of Valsalva.
Reported cases and outcomes of ruptured SVA complicated by preoperative circulatory collapse or cardiac arrest
| Author . | Year published . | No of Pts . | Age . | Diagnosis . | Surgical intervention . | Cause of death . | Outcome . |
|---|---|---|---|---|---|---|---|
| Munk et al. | 1999 | 1 | 35 years | Ruptured SVA | – | Cardiac tamponade | Died preop |
| Doevendans et al. | 2001 | 1 | 67 years | Ruptured SVA | Repair of SVA | Cardiac tamponade | Died postop |
| Lee et al. | 2013 | 1 | 39 years | Ruptured SVA | Repair of SVA | AMI | Died postop |
| Liu et al. | 2014 | 1 | 17 years | Ruptured SVA | – | MOF | Died preop |
| Gilbert et al. | 2017 | 2 | 9 months | Pseudoaneurysm of SoV | – | Cardiac tamponade | Died preop |
| 13.5 months | Pseudoaneurysm of SoV | – | Arrhythmia possibly complicating sepsis | Died preop | |||
| Present case | 2020 | 1 | 27 years | Ruptured of SVA | Repair of SVA and VSD closure | – | Survived |
| Author . | Year published . | No of Pts . | Age . | Diagnosis . | Surgical intervention . | Cause of death . | Outcome . |
|---|---|---|---|---|---|---|---|
| Munk et al. | 1999 | 1 | 35 years | Ruptured SVA | – | Cardiac tamponade | Died preop |
| Doevendans et al. | 2001 | 1 | 67 years | Ruptured SVA | Repair of SVA | Cardiac tamponade | Died postop |
| Lee et al. | 2013 | 1 | 39 years | Ruptured SVA | Repair of SVA | AMI | Died postop |
| Liu et al. | 2014 | 1 | 17 years | Ruptured SVA | – | MOF | Died preop |
| Gilbert et al. | 2017 | 2 | 9 months | Pseudoaneurysm of SoV | – | Cardiac tamponade | Died preop |
| 13.5 months | Pseudoaneurysm of SoV | – | Arrhythmia possibly complicating sepsis | Died preop | |||
| Present case | 2020 | 1 | 27 years | Ruptured of SVA | Repair of SVA and VSD closure | – | Survived |
AMI, acute myocardial infarction; MOF, multiple organ failure; Postop, postoperative; Preop, preoperative; Pt, patient; SoV, sinus of Valsalva.
Percutaneous closure of ruptured SVA has been recently reported, suggesting its viability as a less invasive treatment option. However, it is not suitable for ruptured SVA with associated pathologies (VSD in our patient), which require additional surgical intervention, or with ruptures of a large size [9, 10]. Furthermore, open heart surgery has a higher probability of successful repair of the SVA rupture and other anomalies can be dealt with more easily. In this case, we were obliged to select open surgery due to the patient’s critical condition and the time factor. Our patient recovered with no residual shunt and without other cardiac problems despite her long hospital stay.
In summary, as reported in contemporary medical literature, the outcomes of ruptured SVAs presenting with circulatory collapse or preoperative cardiac arrest are poor with little to no chance of survival. Our case is indeed a rare case of survival, despite the cardiac arrest and multiple organ dysfunction. We believe that the timely surgical intervention altered the expected dismal outcome dramatically.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
Written consent was obtained from the patient.
References
- cardiopulmonary resuscitation
- cardiac arrest
- nitric oxide
- heart diseases
- aneurysm
- cardiogenic shock
- heart failure
- sinus of valsalva aneurysm
- ventricular septal defect
- hemofiltration
- postoperative care
- preoperative care
- rupture
- surgical procedures, operative
- survivors
- tracheostomy
- multiple organ dysfunction syndrome
- sinus of valsalva fistula



