-
PDF
- Split View
-
Views
-
Cite
Cite
Julie Syltern, Geir Jørgensen, Jarle Norstein, Knut Magne Augestad, Fracture and embolization of an implantable venous access device in patient with atrial septal defect, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa548, https://doi.org/10.1093/jscr/rjaa548
Close - Share Icon Share
Abstract
Totally implantable venous access devices (TIVADs) are frequently used for the administration of chemotherapy or parenteral nutrition and have proved to be safe and improve patient quality of life during treatment. Catheter-related infections are the most common complication, whereas catheter fracture and embolization is rarely seen. We present a case of a 61-year-old cancer patient in which the TIVAD fractured and embolized to the patient’s left knee 18 months after its initial placement. An endovascular procedure with intraoperative imaging revealed that the catheter had embolized to the popliteal artery and was successfully removed, the only explanation being the presence of an atrial septal defect. A bubble echocardiogram was unsuccessful in confirming the diagnosis. The catheter fracture could be related to an intravascular procedure that was performed 18 months prior to remove fibrin sheaths as a cause of port malfunction, or it could be a case of pinch-off syndrome.
INTRODUCTION
Totally implantable venous access devices (TIVADs) have been indispensable in the treatment of patients requiring long-term parenteral nutrition or chemotherapy since it was first introduced in the early 1980s. The catheter is implanted using the Seldinger technique, between the clavicle and the first rib, into the subclavian vein, with the tip targeting the right atrium. The catheter is then tunneled and connected to a reservoir that is placed subcutaneously on the upper part of the chest. In the ideal course of treatment, the TIVAD improves quality of life by reducing stress related to repeated venous access procedures, prevents venous toxicity by chemotherapy agents and allows for natural movement in daily life activities. Nonetheless, there are complications related to the use of TIVADs. Premature catheter removal rate is 9.8% where infections are the cause in 80% of the cases [1]. Catheter fracture and embolization is a rare, but potentially serious complication and thus early identification is of vital importance. Where previous case reports of TIVAD fractures describe catheter embolization to the heart and pulmonary vessels [2, 3]; in this article, we present a case of catheter fracture with atypical embolization.
CASE REPORT
A 61-year-old male patient was diagnosed with inoperable stomach cancer. A TIVAD of the type Braun Celsite ST301® was inserted in the right subclavian vein for administration of chemotherapy. Location was confirmed by chest X-ray and the TIVAD was reported functioning with good backflow (Fig. 1). During initiation of the chemotherapy treatment, the TIVAD was reported malfunctioning. Contrast X-ray showed fibrin sheaths at the distal end of the catheter. An endovascular procedure was performed by an interventional radiologist and fibrin sheaths were mechanically removed with a snare (Fig. 2). Intraoperative X-ray with contrast showed normal contrast accumulation distal to the catheter tip and the patient received the first dose of chemotherapy. One month later the patient was hospitalized with bilateral pulmonary thromboembolism. The patient was treated with low-molecular-weight-heparin and discharged. The chemotherapy treatment continued as scheduled, with one pause due to a fracture of the right humerus after a fall. Occasionally, the TIVAD was malfunctioning and medication was administered using a peripheral venous catheter. During a planned pause in treatment, the patient sought hospital care due to worsening of his general condition. CT showed progress of malignancy and another round of chemotherapy was initiated and administrated using the TIVAD without any problems. Less than a week after, the patient reported feeling a tender swelling underneath his left foot. Ultrasound showed no DVT. The swelling and tenderness disappeared spontaneously, but the patient reported brief incidents of pain under his left foot. A CT scan was performed the next time the TIVAD did not function, showing that the distal 8 cm of the catheter was missing. The patient had no symptoms and reported no discomfort of any kind. The TIVAD was removed, confirming a fracture. A chest CT showed no foreign bodies. A full-body CT scan without contrast was performed, revealing the missing catheter part located at the level of the left knee (Figs 3 and 4). Vascular surgeons performed an endovascular procedure through the femoral vein assuming the catheter had embolized to the popliteal vein. Contrast examination revealed no catheter in the vein and another approach through the femoral artery was made, where contrast imaging shows that the catheter was, in fact, located in the popliteal artery (Fig. 5). The catheter, measuring 7.5 cm, was successfully removed with the use of a snare without any complications. The patient was discharged from hospital and referred to a diagnostic echocardiogram (Fig. 6). A bubble echocardiogram was performed to detect an atrial septal defect but was unsuccessful in doing so. For a final diagnosis, the patient was recommended a transesophageal echocardiogram, but as the diagnosis would not alter the course of treatment, the patient declined further examinations. Except for the reported episodes of pain and swelling of the left foot, the patient suffered no injury and finished his chemotherapy treatment.

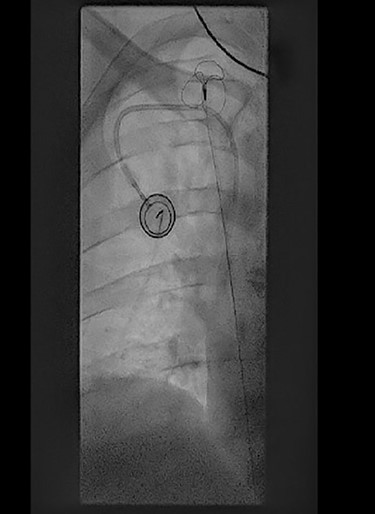
Perioperative fluoroscopy during removal of fibrin sheaths with a snare.
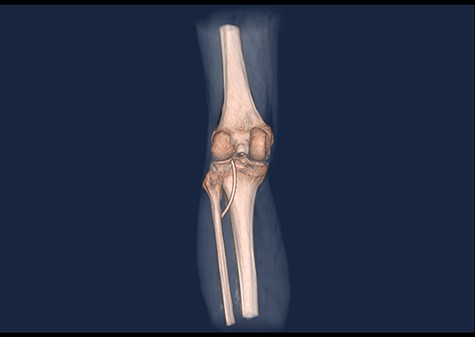
3D CT scan showing posteroanterior view with catheter embolus in the level of the left knee.
DISCUSSION
A systematic review in the pediatric population showed that TIVAD had the lowest rates of failure and complications compared with other central-venous access devices [4]. Pinch-off syndrome (POS) is a well-described cause of catheter fracture, counting for ~40% of the cases [5]. POS is defined by a visible narrowing of the catheter lumen on chest X-ray and is a complication due to mechanical strain on the catheter between the clavicle and the first rib when the catheter has been inserted into the subclavian vein too far medially [5–8]. Another frequent location for catheter fracture is in the proximal part, in the junction between the injection port and the catheter [9]. In 19% of cases, the cause of catheter embolization could not be identified. Duration of catheter placement and line complications such as blockage are also associated with catheter fractures [4]. Clinical presentation of catheter fracture includes catheter malfunction, arrythmias and pulmonary symptoms, but ~25% can be asymptomatic and thus medical professionals should be aware of this complication. The most common sites of fragment embolization are the pulmonary arteries, the right atrium, the right ventricle, the superior vena cava or peripheral veins [2]. In this case, POS was not diagnosed. One may suspect a trauma to the catheter during an endovascular procedure, but the relation remains unclear as it was performed 18 months prior to the incident. The importance of the trauma related to the fracture of the right humerus is also to be considered, but also occurred over a year prior to the catheter fracture. We conclude that in cases of port malfunction, patients should be followed closely to early detect POS or other risk factors such as physical traumas or history of endovascular procedures that are thought to increase the risk of catheter fracture and embolization. Although catheter fracture and embolization is well known in the literature, to our knowledge, this is the first case describing migration of a catheter from the venous side, through an atrial septal defect to arteria poplitea.


Perioperative contrast imaging showing the popliteal artery (black arrow) and the posterior tibial artery (green arrow) with the tip of the catheter embolus in the anterior tibial artery (red arrow).

Perioperative image of percutaneous removal of the catheter using a snare.
ACKNOWLEDGMENTS
The authors would like to recognize the invaluable assistance provided by the Department of Radiology at Helgeland Hospital Trust, and Lars Jakob Hope Rydsaa, M.D. especially, in producing the radiographic images.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



