-
PDF
- Split View
-
Views
-
Cite
Cite
Kelvin Adasonla, Joseph Gabriel, Mohammed Kamil Quraishi, Graham Watson, Massive inguinoscrotal herniation of the bladder: challenges in non-operative management, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa540, https://doi.org/10.1093/jscr/rjaa540
Close - Share Icon Share
Abstract
Massive inguinoscrotal hernias containing the bladder are rare but can present with significant complications such as obstructive uropathy and urinary sepsis. A comorbid 71-year-old gentleman presented with an enlarging inguinoscrotal mass and an acute kidney injury (AKI). Imaging revealed a large inguinoscrotal hernia containing the bladder, and bilateral hydronephrosis. Renal function improved on urethral catheterization. Admitted under general surgery originally, the patient declined any surgical intervention and had his catheter removed as an outpatient, without urological follow up. He represented 6 months later with urinary sepsis and a new AKI. Repeat imaging revealed a progression of the bilateral hydronephrosis. Subsequently admitted under urology, bilateral nephrostomies as well as a catheter were inserted. Once stable, he was discharged with both as part of his long-term management. Non-operative management of this condition may occasionally be necessary, and so requires effective multidisciplinary decision making. Real-world organizational and geographical factors contributed to the challenges in this case.
INTRODUCTION
The urinary bladder is thought to be involved in 1–4% of all inguinal hernias [1]. Cases where a significant portion of the bladder is involved were first described as a ‘Scrotal Cystocele’ by Levine in 1951 [2] and are often referred to as massive or giant. They are associated with a number of complications, including renal impairment, sepsis, strangulation and malignancy [1].
Hernia repair may be challenging in this typically co-morbid population. Non-operative management is therefore necessary in some cases, yet there is a paucity of supporting evidence in the literature. Here we report our experience, highlighting the challenges and learning points in an atypical clinical scenario.
CASE REPORT
A 71-year-old man with a body mass index of 48, history of ischaemic heart disease and bilateral leg ulcers presented to the emergency department with a decline in mobility and worsening scrotal swelling over a year. He described having to compress the scrotal mass to toward the end of urination to complete voiding.
On examination there was significant scrotal swelling, larger on the right-hand side, with a buried penis and both testes impalpable. It was not possible to palpate above the mass in the scrotum. There was erythema and oedema of the scrotal skin, but there were no systemic signs of sepsis or features of Fournier’s gangrene.
Serum laboratory tests on admission revealed a normal white cell count of 10.0 × 109/L, a mildly elevated C reactive protein (CRP) of 34 mg/L and an acute kidney injury (AKI) with a creatinine of 173 μmol/L (baseline 89 μmol/L).
Computed tomography (CT) scan of the abdomen and pelvis with contrast revealed a large right indirect inguinal hernia containing a significant portion of the bladder within the scrotum (Figs 1–3). There was associated bilateral hydronephrosis and hydroureter, and significant scrotal oedema seen within the soft tissues.
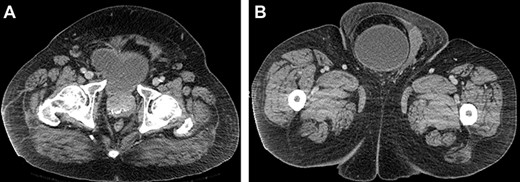
(A and B) Axial CT images of the abdomen and pelvis demonstrating the bladder herniating out of the inguinal canal into the scrotum.

Coronal CT image of the abdomen and pelvis demonstrating herniation of the bladder through the inguinal canal into the scrotum, with associated oedema of the scrotal soft tissues.

Sagittal CT image of the abdomen and pelvis demonstrating herniation of the bladder into the scrotum.
The patient was admitted under the general surgeons given the primary diagnosis was of an inguinoscrotal hernia. A course of intravenous antibiotics was prescribed as per local guidelines for scrotal cellulitis. Following discussion with urology, a urethral catheter was inserted. Renal function improved following catheterization, with creatinine reducing to 83 μmol/L on discharge. Percutaneous nephrostomy insertion was not arranged.
The patient was offered hernia repair, but declined this, citing his poor state of health as the main reason. Following completion of the antibiotic course, he was discharged with an indwelling catheter. He passed a subsequent trial without catheter in the community and was scheduled for a routine outpatient appointment to discuss ongoing surgical management.
The patient presented again to the emergency department 9 months later, complaining of lower abdominal pain. He was pyrexial on admission with a CRP of 201 mg/L, as well as an AKI with creatinine having risen to 481 μmol/L. He was managed as per local protocol for urinary sepsis, and a repeat CT scan was arranged. This revealed a progression of the bilateral hydronephrosis, as well as the persistent hernia. He was admitted under urology on this occasion.
The patient was again catheterized, which did not improve renal function, and so on this occasion had percutaneous nephrostomies inserted during admission. His serum creatinine improved following this, to a new baseline of 170 μmol/L. After again declining operative repair, he was advised that he required long term catheterization and upper urinary tract diversion. He is being followed up with regular changes of both.
DISCUSSION
Given that no widely accepted definition exists, it is difficult to accurately estimate the incidence of giant or massive inguinoscrotal bladder hernias. For the purposes of our paper, we use the definition suggested by Westera et al. [3], where at least 50% of the bladder is found to be inside the hernia sac.
Patients may present with a large inguinoscrotal mass and describe ‘two stage’ urination, where initial spontaneous voiding is followed by manual compression of the hernia to empty the bladder [4]. Herniation of the bladder may compress the bladder trigone or distal ureters, causing an obstructive uropathy and renal impairment, as in our case [4]. A degree of chronic urinary retention is also expected, predisposing patients to urinary tract infection (UTI).
Diagnosis is primarily made with CT scanning [5]. Hernia repair requires initial reduction of the bladder back into its anatomical position, followed by a standard herniorraphy technique [1]. Repair is typically performed open, but both conventional laparoscopic and robotic assisted laparoscopic repairs have also been reported [6].
Repair of massive bladder herniation may involve bowel resection and orchidectomy, and can be complicated by abdominal compartment syndrome, wound dehiscence and hernia recurrence [7]. Given this patient’s frailty, it is understandable that he elected for non-operative management.
This case also highlights the challenges associated with interdisciplinary management of complex patients. The authors speculate that if care between general surgery and urology had been more coordinated, the urethral catheter may never have been removed, perhaps avoiding the subsequent emergency admission. The two departments are separated by an hour’s car journey, yet still belong to the same healthcare institution, or ‘Trust’, and so are expected to deliver effective multidisciplinary care. This is a situation common to many parts of the United Kingdom. Closer monitoring of renal function and elective percutaneous nephrostomy insertion may have been arranged with more adequate integration of care.
Ongoing management in such cases involves further challenges to the urologist. Long term urethral catheterization is associated with UTI, catheter blockage, urethral and penile complications [8], but intermittent self-catheterization or suprapubic catheterization were not feasible in this patient. Similarly, percutaneous nephrostomies may become dislodged or obstructed and require regular exchange [9]. Again, alternatives would bring their own challenges: both retrograde ureteral and extra-anatomic stenting would be technically difficult in this instance.
This is a case report of a rare and extreme variant of a common surgical problem, made more challenging as definitive management was not an option. Crucially, it exemplifies the everyday difficulties in multidisciplinary care and the importance of effective communication between surgical specialties.
CONFLICT OF INTEREST STATEMENT
None declared.
PATIENT CONSENT
Written informed consent for publication of their details was obtained from the patient.



