-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Ho, Thanh Ha Thy Phan, Ralph Jasper Mobbs, Rajesh Reddy, The use of radiolucent (carbon fibre-reinforced polymer) pedicle screw fixation for serial monitoring of clear cell meningioma: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa510, https://doi.org/10.1093/jscr/rjaa510
Close - Share Icon Share
Abstract
Clear cell meningioma is an uncommon variant of meningioma associated with high rates of local recurrence and metastasis. However, monitoring for local recurrence may be complicated by metal-related artefacts generated by spinal instrumentation. We present a patient with recurrent lumbar atypical clear cell meningioma, which had been resected multiple times throughout her adolescence. Due to extensive bone and ligament resection, posterior stabilization of the lumbar spine with pedicle screws was required. To ensure clear postoperative visualization of the spinal cord for local recurrence, a carbon fibre/polyetheretherketone (CF/PEEK) pedicle screw and rod construct was used. CF/PEEK has non-inferior biomechanical and biocompatible properties to titanium, with a clear advantage of radiolucency to assist in detecting the local recurrence early and facilitating accurate radiotherapy planning.
INTRODUCTION
In spinal oncology, there is significant benefit for the development and implementation of radiolucent implants. Metallic implants generate streaking artefacts on computed tomography (CT) and signal loss on magnetic resonance imaging (MRI), which distort the appearance of the spine and impair accurate tumour delineation in postoperative monitoring or radiotherapy planning [1]. Radiolucency allows earlier detection of postoperative complications and local recurrence, which can significantly impact the patient’s quality of life and future treatment decisions. Carbon fibre/polyetheretherketone (CF/PEEK) is a relatively novel material that offers an ideal balance of radiolucency and biomechanical properties suited for tumour applications [2]. Reinforcement of polyetheretherketone by carbon fibre increases its rigidity and elastic modulus closer to bone, reducing the risk of hardware failure while avoiding artefact generation on imaging [3].
The existing literature surrounding the safety and efficacy of CFRP pedicle screws is limited but positive [4, 5]. This case study explores the importance of serial monitoring of a spinal tumour for local recurrence, which is not easily facilitated by standard titanium pedicle fixation.
CASE
A 19-year-old female with a background of a World Health Organization Grade II atypical clear cell meningioma presented with poor mobility, requiring wheelchair assistance, progressive cauda equina symptoms, lower limb numbness and severe radicular leg and hip pain. Two months prior, she was ambulatory and could pass urine without catheterization. Initial resections at age 2, then 4 months after, followed by radiotherapy at age 3 due to subtotal resection were associated with intermittent bladder and bowel dysfunction and long-standing foot drop throughout her childhood. Two years ago she underwent L2–S1 pedicle screw fixation with CF/PEEK screws and rods, with further intradural resection due to recurrence of symptoms. Histopathology of the resected tumour was inconclusive.
Subsequent imaging demonstrated an intradural tumour spanning L1–L5 vertebral levels, involving the conus and lower sacral nerves (Fig. 1). She underwent resection of the tumour, followed by T12 and L1 laminoplasty and revision of her previous L2–S1 fusion. T12–S1 was exposed, and previous CF/PEEK pedicle screws from L2 to L4 were removed. A T12 and L1 laminectomy was performed, with posterior elements preserved for re-implantation. However, it was decided that the laminae would be replaced with CF/PEEK pedicle screws as well. A midline durotomy was made, and an arachnoid specimen was sent for histopathological analysis. The tumour was removed piecemeal with sacrifice of several nerve roots.
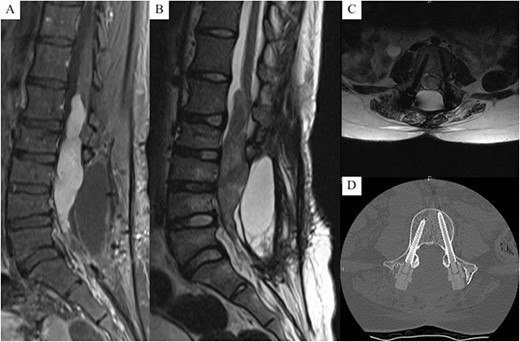
(A) T1 with contrast mid-sagittal MRI, (B) T2 mid-sagittal MRI, (C) T2 axial MRI at L4, (D) axial CT at L4 (bone window), demonstrating a L1 - L5 intradural tumour with significant cauda equina compression; no signal interference or artefacts from the screw construct are present, allowing clear visualisation of the vertebral body and canal.
Postoperative complications included a surgical site infection and acute pain crisis, which were managed appropriately; she recovered with spinal rehabilitation. Ongoing issues include bilateral leg weakness at 3/5 on the Medical Research Council muscle strength scale.
Histopathological analysis suggested malignant peripheral nerve sheath tumour (MPNST) rather than recurrence of her previous meningioma. No further treatment is planned, although the risk of the tumour recurrence remains.
DISCUSSION
Clear cell meningioma is a rare meningioma subtype that occurs in younger patients, and it is more aggressive and likely to metastasize. The local recurrence rate is approximately 60%, hence ongoing monitoring is necessary [6]. MRI is the imaging modality of choice for the evaluation of a spinal cord tumour, allowing good delineation of the spinal cord and cerebrospinal fluid within the vertebral canal.
Surgical management in young patients aims to achieve macroscopic tumour clearance and to preserve the spinal stability [7]. Given the extent of the tumour, significant bone and ligament resection was necessary for complete macroscopic removal. Stabilization with pedicle screw fixation was indicated, given the extent of disease burden and post-tumour resection instability.
Titanium is the predominant material used to manufacture the current pedicle screw and rod constructs, superseding stainless steel. Although there is reduced MRI compared to stainless steel, any artefact is problematic in the postoperative monitoring of a cancer patient as it can impair the clear view of critical anatomical structures. The radiolucent and non-magnetic properties of CF/PEEK make it a useful alternative, especially important where an accurate, unobstructed view of the spine is required to detect the tumour recurrence early and to plan management accordingly. In this case, no artefact from the construct extended to the spinal canal, which allowed the superior and inferior extents of the tumour to be accurately delineated when planning for surgical resection.
For clear cell meningioma, an artefact-free visualization of the spinal canal on MRI allows an easier and earlier detection of local recurrence and/or cerebrospinal fluid seeding. Metallic implants cause artefact on MRI, with the severity being proportional to its magnetic properties. Metal creates static magnetic field inhomogeneity, which alters the phase and frequency of spin in the surrounding tissue [8]. This results in geometric distortion and signal loss within the implant and surrounding tissue [8]. Poor visualization of the spinal cord may result in local recurrence not being detected until there are clinical symptoms.
Postoperative radiotherapy is recommended in treating intraspinal meningioma and MPNST [9], although it may not be indicated if a complete macroscopic resection was achieved and is generally avoided in young patients [9]. Radiotherapy for intradural tumours is complicated by the high risk of radiation myelopathy. Minimizing dose perturbation and scattering is critical when radiotherapy aims to treat to tissue tolerance. Additionally, metal-induced beam scattering and hardening alters the detected CT–Hounsfield units (CT–HU), leading to inaccuracies in estimating the dose drop off. One of CF/PEEK’s biggest advantages is its compatibility with radiotherapy planning and delivery. Because the CT–HU of CF/PEEK is close to physiological values, dosage planning algorithms better predict the radiation absorption and scatter. The CT–HU of titanium often exceeds the capability of these algorithms, increasing the uncertainty in dose delivery. Ringel et al. [3] reported a significant mean reduction in the artefact volume of almost 50% with CF/PEEK screws compared to equivalent titanium screws, allowing a more accurate delineation of tumour from the normal structures when contouring a target planning volume.
CONCLUSION
We present a rare case of malignant clear cell meningioma with multiple recurrences over the patient’s life. Given the invasive and malignant nature of the tumour, repeated radiotherapy and surveillance is necessary, especially as the patient is young. CF/PEEK pedicle screws were preferred as they allow an unimpeded visualization of the vertebral column and spinal canal on CT and MRI and enhance the radiotherapy delivery.
AUTHORS’ CONTRIBUTIONS
D.H. and T.H.T.P. obtained the patient information and wrote the manuscript. R.J.M. and R.R. provided the administrative and editorial inputs for the manuscript.
CONSENT
The patient has provided informed consent for her details to be included in this case report.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



