-
PDF
- Split View
-
Views
-
Cite
Cite
Omar Ahmed, Sara Mahmood, Youssef Aladham, Moustafa Mohamed Abdelnaby, Traumatic pseudoaneurysm of the cavernous carotid: a lethal complication of craniofacial trauma, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa500, https://doi.org/10.1093/jscr/rjaa500
Close - Share Icon Share
Abstract
Pseudoaneurysm of the cavernous carotid artery is a rare, yet life-threatening complication of craniofacial trauma. It may well present itself with delayed massive epistaxis up to several months after the initial insult. Early recognition and prompt treatment are the key in management and a high index of clinical suspicion is always required. In this article, we report a patient with a penetrating head injury who developed delayed epistaxis along with unilateral abducent and partial oculomotor palsy. Urgent diagnostic carotid angiography was undertaken, followed by endovascular coiling that resulted in no recurrence for a year of follow-up.
INTRODUCTION
Post-traumatic pseudoaneurysm of the cavernous carotid artery (CCA) poses a challenge in its diagnosis and treatment [1]. It is a rare, yet life-threatening cause of epistaxis and a high index of suspicion is required for rapid recognition and optimum management. Those false aneurysms have a fibrous wall surrounding a hematoma that intermittently ruptures giving rise to massive bleeding episodes [2]. The time between the traumatic event and the onset of bleeding considerably varies from a few days to several weeks, which as such adds to its diagnostic dilemma [3]. Clinically, a triad of recent head trauma, acute unilateral eye symptoms and intermittent profound epistaxis should raise the suspicion of CCA pseudoaneurysm and warrant urgent angiographic evaluation [4]. Treatment strategies include parent artery occlusion along with reconstruction of the circulation surgically or via endovascular techniques [5].
CASE PRESENTATION
A 23-year-old female patient presented to the outpatient clinic with a two-month history of recurrent attacks of severe epistaxis mainly from the right nostril. Though the amount of blood loss was significant, its frequency varied. This had been usually initiated by cough, straining, leaning forward and sexual intercourse and ceased spontaneously. She denied any other nasal symptoms.
Her medical history revealed a previous high dependency unit (HDU) admission for observation 6 months earlier after a gun pellets injury in the head and neck region. She was completely asymptomatic at that time; however, she admitted that she suffered from double vision two months after she was discharged.
Nasal endoscopy was unremarkable apart from a small blood clot seen in the right sphenoethmoidal recess. Further examination displayed right convergent squint, ptosis and miosis.
Computed tomography (CT) of the paranasal sinuses and angiography were requested on an urgent basis, which confirmed a diagnosis of pseudoaneurysm in her right CCA, adjacent to retained pellets (Figs 1–4). Also, her hemoglobin dropped from 11.5 to 8.4 gm over a 6-month period. Afterwards, she was referred to the interventional radiology department. She underwent stenting and coiling of her right internal carotid artery after which no further epistaxis happened for an uneventful year of follow-up.
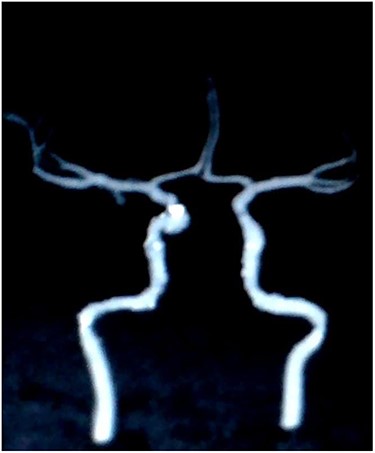
Digital subtraction carotid angiography showing small hyperdense area in the right cavernous carotid artery.

CT scan coronal view showing gun pellets near the right cavernous carotid artery (arrows).
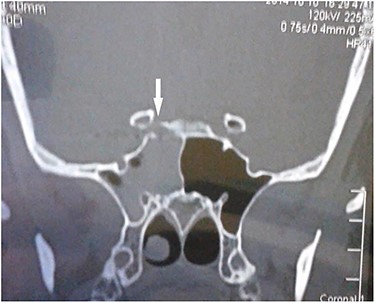
CT scan coronal view showing right sphenoid sinus opacification with denudation of sphenoid sinus wall (arrow).
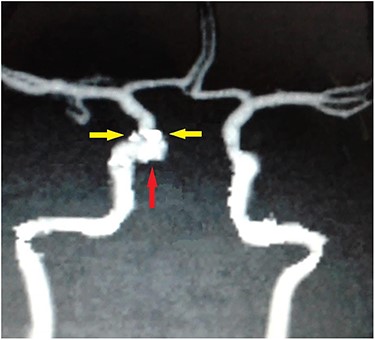
Carotid angiography showing small gun pellets (yellow arrows) and pseudoaneurysm (red arrow) of the right CCA.
DISCUSSION
Traumatic intracranial aneurysms are considered rare (<5% of all intracranial aneurysms) [6]. They mostly arise within the anterior circulation (90%). Penetrating trauma accounts for almost 40% of traumatic pseudoaneurysms that arise within the posterior circulation [7]. Traumatic aneurysms are essentially pseudoaneurysmal in nature, wherein penetrating injuries cause direct vessel wall injury resulting extravasation of blood within a capsule of fibrous connective tissue and producing a contained, throbbing hematoma [2].
The anatomical relationship between the CCA and the sphenoid sinus has been well described in literature. Renn and Rhoton [8] concluded that the internal carotid artery (ICA) bulges into the sphenoid sinus in 71% of their specimens, and are usually covered by a thin bony layer (<1 mm thick in 66%); 4% of cases had no bony layer and were only covered by sinus mucosa. Pulsatile forces of an aneurysm in the CCA may result in the erosion of the thin bony layer that separates it from the sphenoid sinus resulting in hemorrhage into the sinus [9]. This was demonstrated in the case described above, where compression of the oculomotor and abducent nerve within the cavernous sinus leads to the findings of ptosis, miosis and convergent squint. The timeframe between the traumatic incident and the presentation of a traumatic pseudoaneurysm in any form can vary from days to weeks (average of 3 weeks in 88% of cases) [3]. It was found to be 6 months in our case. This delayed presentation could be explained by the time interval between the traumatic event weakening the vessel wall and for the pulsatile pressure to erode into the thin bony wall around the cavernous sinus. The first episode of epistaxis may not be severe and may be disregarded by the patient or the primary health carer, which would result in further delay.
CCA pseudoaneurysm rupture causing epistaxis is rare and pose a mortality risk of 30–50% [6]. If a clinical suspicion arises in a case presenting with intractable epistaxis, angiography becomes an essential tool for diagnosis and management as prompt diagnosis can significantly reduce mortality. Intra-arterial digital subtraction angiography is the diagnostic modality of choice as it also helps with definitive management planning [3]. Alternatively, CT angiography or magnetic resonance angiography can be used, but they both have the disadvantage of limited demarcation of cross-circulation.
Accepted treatment strategies include surgical and endovascular techniques. While surgery is the ideal management, direct surgical exposure of the cavernous ICA is challenging. Carotid artery occlusion or surgical ligation has also been described, but that poses the risk of significant cerebrovascular events even with patent cross-circulation. There also remains the risk of development of collateral blood flow to the pseudoaneurysm leading to recurrence [5].
Endovascular approaches for management of traumatic pseudoaneurysms presenting with intractable epistaxis are gaining increased popularity nowadays and carry lower complication rates. Lampert et al. [10] described safe and successful direct coiling of eleven consecutive post-traumatic pseudoaneurysms with parent vessel preservation. The nature of pseudoaneurysm makes tight coiling quite problematic as it consists only of fibrous tissue and has no true wall to confine the coil as opposed to true aneurysms. In the case above, we were able to isolate and obliterate the pseudoaneurysm using stent-assisted coils.
In conclusion, epistaxis is a common serious condition. It is fundamental to include traumatic pseudoaneurysm in the differential diagnosis of intractable epistaxis, especially in the presence of any head injury regardless of the delay in presentation. Traumatic CCA pseudoaneurysm can cause massive epistaxis with significant mortality and can be appropriately managed by endovascular techniques, which are relatively safe and potentially lifesaving.
CONFLICT OF INTEREST STATEMENT
The authors state no conflict of interest with regard to the publication of this paper.
FUNDING
The authors state no funding source for this work.



