-
PDF
- Split View
-
Views
-
Cite
Cite
Diogo Belo, Joaquim Cruz Teixeira, José Pedro Lavrador, Postoperative Brown-Séquard syndrome: case report and review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa460, https://doi.org/10.1093/jscr/rjaa460
Close - Share Icon Share
Abstract
Brown-Séquard syndrome (BSS) is a rare neurological condition caused by a hemi-lesion of the spinal cord and was first described in the 1800s. BSS is characterized by an ipsilateral absence of motor control and discriminatory/proprioceptive/vibratory sensation at and below the spinal level involved, associated with loss of contralateral temperature and pain sensation a couple of vertebral segments below the lesion. BSS is commonly associated with trauma, but can also be iatrogenic. The authors report a case of a patient who presented with neoplastic dorsal spinal cord compression and developed a BSS after surgical decompression and review of the literature of postoperative BSS cases.
INTRODUCTION
Spinal cord injury (SCI) can lead to a partial or complete loss of motor, sensory as well as autonomic functions below the level of lesion.
Brown-Séquard Syndrome (BSS) is a rare neurological condition [1] with incomplete SCI.
BSS is well described in the literature and may have two different presentations: a ‘classical’ and more complete presentation and an incomplete presentation, more prevalent than the latter.
The classical syndrome is the consequence of a hemisection of the spinal cord with ipsilateral paralysis and loss of proprioceptive and vibratory sensation on the same side and loss of pain and temperature sensation on the contralateral side [2].
The motor paralysis seen in this syndrome results from disruption of the corticospinal tracts that decussate in the lower medulla, thus, the motor findings are seen on the same side as the injury.
Disruption of the spinal cord causes loss of pain sensation and temperature on the contralateral side, starting one or two levels below the site of the lesion.
Although BSS is a quite recognizable condition, its exact incidence is difficult to determine. ‘Brown-Séquard’-like syndromes, on the other hand, probably account for ~2–4% of all traumatic SCIs.
The authors present a case of postoperative BSS and review of the literature on iatrogenic BSSs.
CASE PRESENTATION
The authors present the case of an 82-year-old man presented to the ED with a progressive paraparesis that started a month before admission. His past medical history was unremarkable.
Neurological examination revealed a symmetric paraparesis (muscle power grade 4/5) below the T5 spinal cord segment. Babinski reflex and ankle clonus were present and both touch, pain, thermal and tactile sensations were preserved.
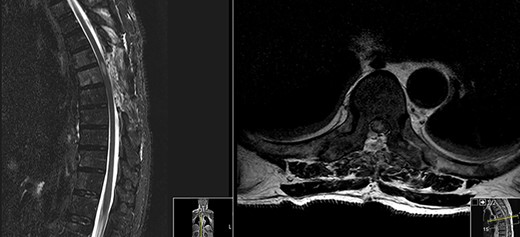
Spinal magnetic resonance imaging (MRI) (Fig. 1) showed an hyperintense contrast-enhancing abnormal mass at the level of T6 which occupied the left side of the spinal canal and compressed the spinal cord.
Further investigation revealed multiple metastatic lesions and prostate cancer as the probable primary neoplastic site.
The patient underwent a T5-T7 laminectomy and complete removal of epidural tumoral mass.
On Day 2 post-op, the patient developed a right-sided BSS (right leg monoplegia and ipsilateral tactile, epicritic and proprioceptive hyposthesia below T5 and thermal and pain left-sided anesthesia).
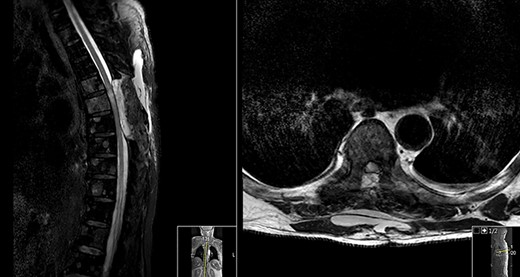
Postoperative MRI (Fig. 2) revealed a de novo T2 hyperintensity, possibly due to retraction of the thecal sac during surgery and consequently spinal cord lesion.
| Reference . | Medical field . | Surgical technique . | BSS cause . | Onset . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Horowitz et al. [7] | Spine Surgery | Laminectomy | Radiculomyelopathy caused by pseudomeningocele | Delayed | Spontaneous resolution after 3 months | Full recovery |
| Praharaj et al. [8] | Spine Surgery | Cervical Laminoplasty | Under riding of the lamina on the hinged side at C3 level | Immediate | Laminectomy | Improvement of the motor power |
| Yamazaki et al. [9] | Spine Surgery | Laminectomy + posterior instrumented fusion | Decompression procedure itself | Immediate | Methylprednisolone | Recovery after 3 months |
| Sucu et al. | Spine Surgery | Cervical pedicle-screw fixation + total laminectomy | Hyperextension and lateral binding of the neck | Immediate | Dexamethasone; Prednisolone | Partial recovery after 18 months |
| Lee et al. | Spine Surgery | C1-C2 fusion | Hyperextension of the neck | Delayed | Conservative treatment | Partial recovery after 8 months |
| Jost et al. | Spine Surgery | C3-C5 Laminectomy | Paraspinal muscles edema + kyphosis | Immediate | Dexamethasone + surgical exploration | Full Recovery after surgery |
| Van Orman et al. | Spine Surgery | Harrington rod instrumentation | Anterior spinal artery or spinal vein damage | Immediate | Conservative treatment | No recovery |
| Wilber et al. | Spine Surgery | Harrington rod instrumentation | Not explained | Immediate | Unknown | Unknown |
| Reference . | Medical field . | Surgical technique . | BSS cause . | Onset . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Horowitz et al. [7] | Spine Surgery | Laminectomy | Radiculomyelopathy caused by pseudomeningocele | Delayed | Spontaneous resolution after 3 months | Full recovery |
| Praharaj et al. [8] | Spine Surgery | Cervical Laminoplasty | Under riding of the lamina on the hinged side at C3 level | Immediate | Laminectomy | Improvement of the motor power |
| Yamazaki et al. [9] | Spine Surgery | Laminectomy + posterior instrumented fusion | Decompression procedure itself | Immediate | Methylprednisolone | Recovery after 3 months |
| Sucu et al. | Spine Surgery | Cervical pedicle-screw fixation + total laminectomy | Hyperextension and lateral binding of the neck | Immediate | Dexamethasone; Prednisolone | Partial recovery after 18 months |
| Lee et al. | Spine Surgery | C1-C2 fusion | Hyperextension of the neck | Delayed | Conservative treatment | Partial recovery after 8 months |
| Jost et al. | Spine Surgery | C3-C5 Laminectomy | Paraspinal muscles edema + kyphosis | Immediate | Dexamethasone + surgical exploration | Full Recovery after surgery |
| Van Orman et al. | Spine Surgery | Harrington rod instrumentation | Anterior spinal artery or spinal vein damage | Immediate | Conservative treatment | No recovery |
| Wilber et al. | Spine Surgery | Harrington rod instrumentation | Not explained | Immediate | Unknown | Unknown |
| Reference . | Medical field . | Surgical technique . | BSS cause . | Onset . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Horowitz et al. [7] | Spine Surgery | Laminectomy | Radiculomyelopathy caused by pseudomeningocele | Delayed | Spontaneous resolution after 3 months | Full recovery |
| Praharaj et al. [8] | Spine Surgery | Cervical Laminoplasty | Under riding of the lamina on the hinged side at C3 level | Immediate | Laminectomy | Improvement of the motor power |
| Yamazaki et al. [9] | Spine Surgery | Laminectomy + posterior instrumented fusion | Decompression procedure itself | Immediate | Methylprednisolone | Recovery after 3 months |
| Sucu et al. | Spine Surgery | Cervical pedicle-screw fixation + total laminectomy | Hyperextension and lateral binding of the neck | Immediate | Dexamethasone; Prednisolone | Partial recovery after 18 months |
| Lee et al. | Spine Surgery | C1-C2 fusion | Hyperextension of the neck | Delayed | Conservative treatment | Partial recovery after 8 months |
| Jost et al. | Spine Surgery | C3-C5 Laminectomy | Paraspinal muscles edema + kyphosis | Immediate | Dexamethasone + surgical exploration | Full Recovery after surgery |
| Van Orman et al. | Spine Surgery | Harrington rod instrumentation | Anterior spinal artery or spinal vein damage | Immediate | Conservative treatment | No recovery |
| Wilber et al. | Spine Surgery | Harrington rod instrumentation | Not explained | Immediate | Unknown | Unknown |
| Reference . | Medical field . | Surgical technique . | BSS cause . | Onset . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Horowitz et al. [7] | Spine Surgery | Laminectomy | Radiculomyelopathy caused by pseudomeningocele | Delayed | Spontaneous resolution after 3 months | Full recovery |
| Praharaj et al. [8] | Spine Surgery | Cervical Laminoplasty | Under riding of the lamina on the hinged side at C3 level | Immediate | Laminectomy | Improvement of the motor power |
| Yamazaki et al. [9] | Spine Surgery | Laminectomy + posterior instrumented fusion | Decompression procedure itself | Immediate | Methylprednisolone | Recovery after 3 months |
| Sucu et al. | Spine Surgery | Cervical pedicle-screw fixation + total laminectomy | Hyperextension and lateral binding of the neck | Immediate | Dexamethasone; Prednisolone | Partial recovery after 18 months |
| Lee et al. | Spine Surgery | C1-C2 fusion | Hyperextension of the neck | Delayed | Conservative treatment | Partial recovery after 8 months |
| Jost et al. | Spine Surgery | C3-C5 Laminectomy | Paraspinal muscles edema + kyphosis | Immediate | Dexamethasone + surgical exploration | Full Recovery after surgery |
| Van Orman et al. | Spine Surgery | Harrington rod instrumentation | Anterior spinal artery or spinal vein damage | Immediate | Conservative treatment | No recovery |
| Wilber et al. | Spine Surgery | Harrington rod instrumentation | Not explained | Immediate | Unknown | Unknown |
No hydrosyringomyelia or other complications were visible.
The patient remained in the ICU for 3 days in order to maintain vasopressor-induced high blood pressure and adequate spinal cord perfusion.
Patient was referred to PT and started his motor rehabilitation program on Day 3 post-op.
Prior to discharge, patient’s strength was grade 1/5 on the right leg and 4/5 on the left leg; he had proprioceptive impairment on both feet and hyposthesia below T5.
Three months after discharge, the patient had partially recovered from the motor deficit on his lower right limb, having a motor strength grade 2/5.
Neurological exam was otherwise unremarkable, having made a full recovery from the sensory deficit and motor deficit on his lower left limb (present preoperatively).
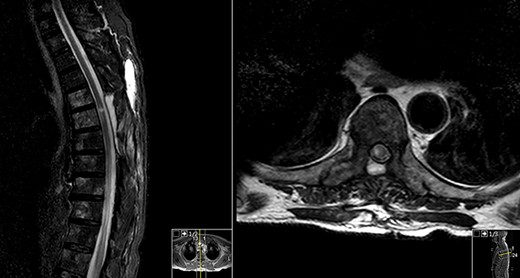
MRI done at this time showed a reduction in the T2 hyperintensity seen in both previous post-op MR scans (Fig. 3).
DISCUSSION
The syndrome was first published by Brown-Séquard in the mid 1800s, where a BSS was described in a patient suffering from a penetrating injury to the spinal cord.
Peacock et al. [3] described a series of 1600 patients with various SCIs, 16% of these (240 patients) had reportedly developed BSS after sustaining similar penetrating wounds.
Traumatic but non-penetrating causes that have been reported include blunt trauma, including atypical disk herniation [4], vertebral fractures or gunshot wounds [4,5].
Most reported cases of BSS after blunt trauma in adults are due to instability of the spine, either a fracture of the bony elements or ligamentous instability. In cases where blunt trauma does not result in a fracture, the proposed mechanism of injury is disc protrusion, vascular compromise, transient subluxation of the vertebral bodies, or stretching of the cord itself [5,6].
Among non-traumatic reported causes we can find arachnoid cysts, syringomyelia, hematomyelia, tumor, epidural hematomas, vasculitis after heroin injection, decompression sickness due to mechanical obstruction of blood flow and meningococcal myelitis.
The development of BBS as a surgical complication is not common.
In fact, most neurological complications of several surgical procedures are generally expressed through paraparesis.
After a literature review, eight published case reports on BSS following a surgical procedure (Postoperative BSS) were found and summarized in Table 1.
Notwithstanding, the majority of cases in which postoperative BSS occurred is predominantly related to three medical fields: vascular surgery, orthopedic surgery and neurosurgery.
In regards to vascular procedures, most BSS situations originated due to ischemia or embolization, whereas on the neurosurgical and orthopedic fields the occurrence of postoperative BSS was mostly caused by compression or direct lesion of the spinal cord.
Regardless of the exact mechanisms (which still warrant more directed research) causing the deficit, the symptoms are mostly reversible, similarly to what is observed in non-iatrogenic BSS.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



