-
PDF
- Split View
-
Views
-
Cite
Cite
Gregory Sigler, Laura Baker, Shaheer Tadros, Janelle Rekman, Sameer S Apte, Acute midgut volvulus in a septuagenarian with secondary jejunoileal diverticulitis and undiagnosed congenital malrotation: an unusual presentation, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa449, https://doi.org/10.1093/jscr/rjaa449
Close - Share Icon Share
Abstract
A 79-year-old male presented with abdominal pain, incidental umbilical hernia and acute midgut volvulus that was not detected until surgical exploration. When he presented to hospital, computed tomography (CT) findings indicated perforated jejunoileal diverticulitis; however, in the operating room clockwise volvulization of the jejunum and ileum, secondarily inflamed jejunoileal diverticula, incomplete malrotation (right-sided duodenojejunal flexure), right retroperitoneal adhesions (Ladd’s bands) and numerous other congenital adhesive bands were found. A modified Ladd’s procedure and umbilical hernia repair were completed including detorsion, division of Ladd’s bands with medialization of the cecum and lysis of other congenital adhesions without appendectomy. The patient recovered to baseline function by 3 weeks postoperatively. Acute midgut volvulus is a life-threatening surgical emergency that is exceptionally rare in the elderly. CT is relatively insensitive, so misdiagnosis is common. A high index of suspicion is required, especially in patients with a history of congenital gastrointestinal abnormalities. Prompt surgical exploration for correction and prevention is crucial.
INTRODUCTION
Acute midgut volvulus is a life-threatening surgical emergency in adults. Incidence is estimated at 0.2% in adults and decreases with age [1, 2]. With a mean age at presentation of 39, midgut volvulus is exceptionally rare in the elderly [3]. If not promptly recognized, it can lead to obstruction, ischemia and death. Due to its rarity and the relative insensitivity of computed tomography (CT), misdiagnosis is common [3, 4]. A high index of suspicion is required, especially in patients with a history of congenital gastrointestinal abnormalities. Prompt surgical exploration for correction and prevention is crucial. Here we present a case highlighting the recognition and management of a unique triad of midgut volvulus, congenital malrotation and secondary jejunoileal diverticulitis in a septuagenarian.
CASE PRESENTATION
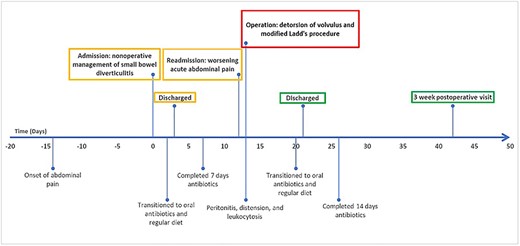
A 79-year-old male presented with 2 weeks of persistent abdominal pain. He did not report any nausea, vomiting or chills. Past medical history included aortic stenosis and type II diabetes, and no history of previous abdominal surgery. His abdomen was soft, non-distended, with mild generalized tenderness and an incidental umbilical hernia. Vitals signs were normal. His white blood cell count was 16.7 × 109/L. CT identified multiple distended and inflamed jejunoileal diverticula. There was no free fluid or gas (Fig. 1). The patient was admitted with small bowel diverticulitis and managed with bowel rest and intravenous antibiotics. He was discharged on post-admission Day 3.
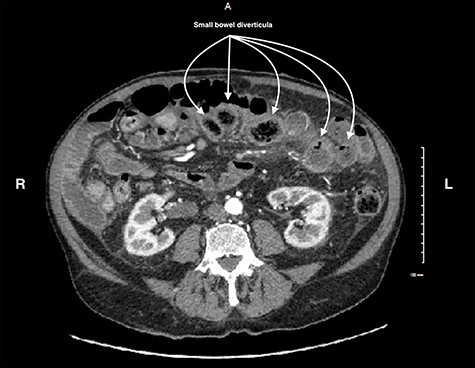
CT scan of the abdomen and pelvis showing small bowel diverticula with inflammation and stranding consistent with uncomplicated diverticulitis.
He presented again on Day 9 with 1 day of recurrent abdominal pain. His abdomen was distended with focal tenderness centrally. Vital signs were normal. White blood cell count was 12.9 × 109/L. Repeat imaging reported multiple inflamed jejunoileal diverticula. There was no free fluid, gas or abscess. He was admitted to hospital for bowel rest and a second course of intravenous antibiotics. On Day 10, he became severely distended with peritonitis. His white blood cell count increased to 22.9 × 109/L. He underwent emergent operative exploration for possible perforated jejunoileal diverticulitis.
Upon entry, numerous, sizable, jejunoileal diverticula were encountered. There was hemorrhagic ascites with no pus or bowel content. There was clockwise volvulus of the proximal ileum, with early signs of vascular compromise. Counterclockwise detorsion was immediately performed. After inspection, congenital malrotation was noted—the duodenojejunal flexure was right-sided, entering the intraperitoneal space just medial to the cecum (Fig. 2). There were right-sided cecal adhesions to the retroperitoneum (Ladd’s bands) and other congenital adhesions from the omentum to the bowel and abdominal wall.
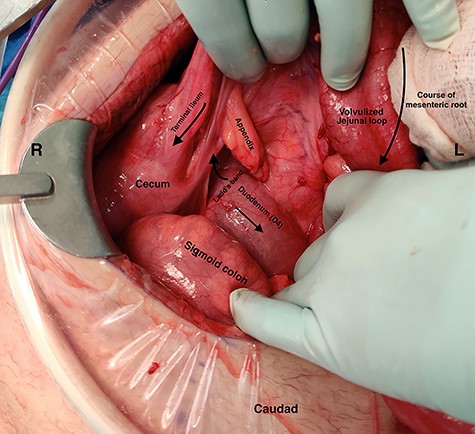
Intraoperative photograph demonstrating: (i) the duodenojejunal flexure entering the intraabdominal space deep to the ileocecal mesentery, on the right side of the abdomen (ii) volvulus of the jejunum around its mesentery (iii) terminal ileum coursing superior to the volvulized jejunum.
Most of the small bowel contained diverticulosis, sparing the proximal jejunum (50 cm) and distal ileum (50 cm) (Fig. 3). There was no primary diverticular inflammation, only secondary inflammation from volvulus. There was no inter-loop purulence to indicate perforation. Manual pressurization of all small bowels underwater revealed no air leak. A modified Ladd’s procedure (without appendectomy) was performed. The Ladd’s bands and all other congenital adhesions were lysed, medializing the cecum. At the conclusion of the operation, the cecum was in a left midline position, and the small bowel mesentery was lengthened and detorted. All small bowels were viable.
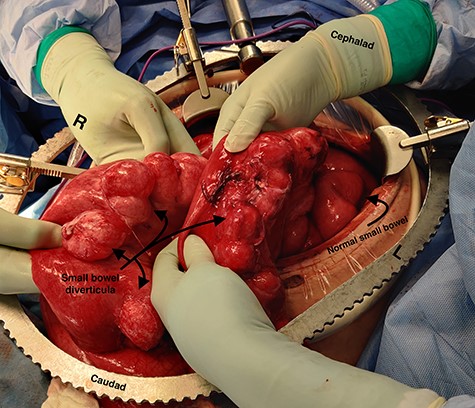
Intraoperative photograph demonstrating extensive small bowel diverticulosis with dilatation of the small bowel secondary to obstruction from midgut volvulus – also visible are segments of normal small bowel.
The patient recovered with bowel rest and antibiotics. Postoperatively, the patient revealed a history of externalized viscera (omphalocele or gastroschisis) as a newborn. He was discharged on postoperative Day 8. Three weeks later, his bowel function and appetite were normal, and he had returned to normal activities of daily life (Fig. 4).
DISCUSSION
Midgut volvulus is an uncommon disease most often presenting in children, with rare occurrences in adults [3]. It is characterized by an abnormal rotation of the intestine around a fixed-point. Associated congenital conditions include gastrointestinal malrotation, jejunoileal diverticulosis and a history of abdominal wall defects [5, 6]. Acutely, volvulus can be intermittent or complete, with variable symptoms, leading to obstruction, bowel necrosis and possibly death. Chronic presentations of midgut volvulus can also occur, resulting in recurrent pain, intermittent obstruction and malabsorption over months to years. Due to its rarity in adults and variable presentation, preoperative diagnosis of intestinal volvulus is challenging. Adding to this difficulty, a classic ‘whirlpool sign’ or abnormal superior mesenteric vessel configuration is only present on CT in 30.9 and 58% of cases, respectively [3]. Retrospectively, the right-sided position of the duodenojejunal flexure and slight swirling of small bowel mesentery is visible but clouded by numerous jejunoileal diverticula (Figs 5 and 6).
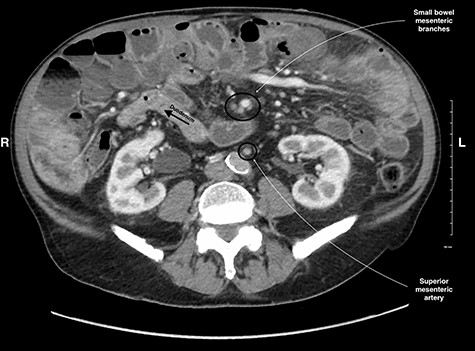
CT image of the right sided position of duodenojejunal flexure, entering the intraperitoneal cavity on the right side of the abdomen.
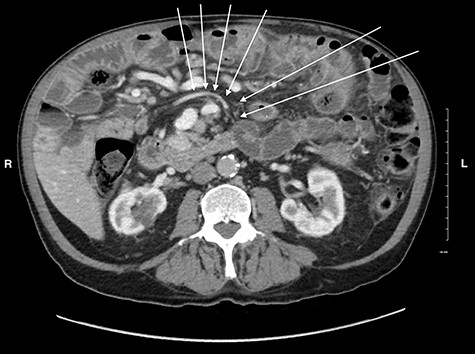
CT image showing a subtle swirl of the mesenteric vein, coursing from the left to the right side of the abdomen indicating volvulus of the small bowel.
Although midgut volvulus in adulthood is unusual, malrotation as an underlying cause is exceptionally rare. A review of the ‘United States Nationwide Inpatient Sample’ by Coe et al. [7] demonstrated that out of 20 868 cases of intestinal volvulus, only 169 (0.82%) were attributable to malrotation. Similarly, Nehra and Goldstein [8] performed a retrospective review of 82 adults diagnosed with congenital malrotation over 20 years at the Massachusetts General Hospital. Nearly 75% of these patients had been experiencing symptoms for months to years, with intermittent abdominal pain as the most common symptom (87%). Only 12% of these patients presented with volvulus. Similarly, Neville et al. reported that 87.6% of adults with malrotation reported chronic symptoms including pain (41%), vomiting (12%) and constipation (12%). Many of these patients eventually presented with acute complications like volvulus, requiring urgent intervention [3].
Increased surgeon awareness of the variability in presentation of volvulus and congenital malrotation may help foster recognition, expedite intervention and improve patient outcomes. In the case presented here, neither malrotation nor volvulus was identified on two preoperative CT scans performed within 12 days.
The link between congenital abdominal wall defects, malrotation and volvulus is well documented [1, 2, 5, 8]. Our patient described a history of congenital abdominal wall defect (likely gastroschisis or omphalocele) consistent with his known umbilical hernia. Recently, Lauriti et al. [5] performed a systematic review and meta-analysis of 3888 infants with omphalocele, revealing an association with malrotation in 3.5% of patients. Concordantly, Fawley et al. [6] found an incidence of intestinal volvulus of 4.4% with omphalocele and 1.9% with gastroschisis in infants. Unfortunately, there are no studies documenting follow-up of children with congenital abdominal wall defects into adulthood. Thus, the incidence of adult-onset intestinal volvulus secondary to congenital malrotation is unknown. Preoperative knowledge of our patient’s congenital abdominal wall defect may have raised suspicion for volvulus as an underlying cause of his abdominal pain.
The traditional Ladd’s procedure, initially described by William Ladd in 1936 to treat intestinal malrotation in infants, includes four key components: (i) detorsion of small bowel volvulus if present, (ii) division of Ladd’s bands, (iii) widening of the root of the small bowel mesentery and (iv) prophylactic appendectomy [9]. Traditionally, appendectomy as a part of Ladd’s procedure is performed in children to avoid future diagnostic confusion due to an abnormally located appendix and significant lifetime risk of appendicitis. For children, CT for possible appendicitis is often avoided, increasing the likelihood of diagnostic uncertainty in these patients. In our case, appendectomy was omitted due to the low likelihood of future appendicitis for a 79-year-old, the desire to avoid unnecessary violation of the viscera when no intestinal resection was needed, and the high likelihood of repeat CT if he presents again with abdominal pain. We propose that the omission of appendectomy is a reasonable modification of Ladd’s procedure for elderly patients.
To our knowledge, no previously documented cases of concurrent acute intestinal volvulus, small bowel diverticulitis and congenital malrotation exist. For elderly patients presenting with acute abdominal pain, surgeons should be aware of the possibility of intestinal volvulus due to congenital malrotation, especially when there is a history of congenital abdominal wall defects.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- abdominal pain
- computed tomography
- appendectomy
- adhesions
- adhesives
- diverticulitis
- diverticulum
- hernia, umbilical
- operating room
- retroperitoneal space
- cecum
- ileum
- jejunum
- malrotation, congenital
- older adult
- repair of umbilical hernia
- cytolysis
- misdiagnosis
- exploratory surgery
- band of ladd
- emergency surgical procedure
- prevention
- undiagnosed



