-
PDF
- Split View
-
Views
-
Cite
Cite
Joanna Chorbińska, Wojciech Krajewski, Maciej Sroczyński, Maciej Guziński, Romuald Zdrojowy, Splenosis mimicking lymphadenopathy, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa425, https://doi.org/10.1093/jscr/rjaa425
Close - Share Icon Share
Abstract
Splenosis is an autotransplantation of splenic tissue following traumatic rupture of the spleen or splenectomy. Generally, splenosis is asymptomatic. Therefore, most cases are incidental findings made during surgery, autopsy or after imaging studies for other purposes. Splenosis is a benign phenomenon, but it often shows similarity to the metastatic process. We present a case of asymptomatic intraperitoneal splenosis occurring in a 57-year-old male, in whom computed tomography urography showed lymphadenopathy suggesting a neoplastic process. A reconnaissance laparotomy was performed, and specimens were taken and sent for histopathological examination. The microscopic image of all the collected lesions corresponded to the normal spleen tissue. Due to an increasing number of traffic accidents, it is worth taking abdominal splenosis into consideration in the differential diagnosis of tumor-like changes, especially in patients with a history of splenic trauma or spleen removal. As a result, unnecessary surgery can be avoided in many cases.
INTRODUCTION
Splenosis is an autotransplantation of splenic tissue following traumatic rupture of spleen or its damage during splenectomy [1, 2]. Abnormalities are usually detected accidentally during imaging studies, autopsy or surgery for another reason [3]. Splenosis is a benign phenomenon, but often shows similarity to the metastatic process. Therefore, making the correct diagnosis is important as it significantly affects further patient management [1, 2].
We present a case of asymptomatic intraperitoneal splenosis occurring in a 57-year-old male, in whom computed tomography (CT)-urography showed lymphadenopathy highly suggestive for a neoplastic process. This atypical diagnosis indicates the need to broaden and disseminate knowledge about splenosis. This will help to avoid skipping splenosis in the differential diagnosis of tumor-like changes revealed in abdominal imaging in a patient after a spleen injury.
CASE REPORT
In April 2018, a 57-year-old man was admitted to the Department of Urology for the diagnosis of left kidney nephrolithiasis and qualification for therapeutic procedures. Apart from renal colic, he had no other symptoms. The patient’s history included chronic hepatitis B, hypertension, left bundle branch block and prostate enlargement. In childhood, he underwent splenectomy after a traffic accident. His physical examination was normal, and routine blood work demonstrated no significant laboratory abnormalities.
After proper preparation, CT-urography was performed. An imaging examination showed a 9 mm stone in the lower calyx of the left kidney. Attention was drawn to numerous pathological lymph nodes up to 3 cm in size, located along the left and right iliac axis, as well as in pelvic peritoneal fat, along the intestinal loops, especially the sigmoid colon and caecum (Fig. 1).
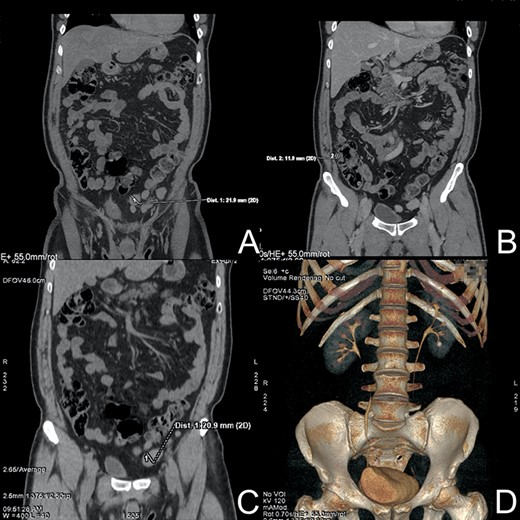
CT-urography. (A) Enlarged lymph node near sigmoid colon. (B) Pathological lymph node near the ascending colon. (C) Low-dose CT without contrast—lymph node. (D) 9 mm stone in the lower calyx of the left kidney.
In June, the patient was admitted to the Department of General, Minimally Invasive and Endocrine Surgery for the reconnaissance laparotomy. During the procedure, a greater omentum with tuberous lesions and similar implants in the peritoneal wall of the pelvis were visualized. The largest conglomerate of changes was sampled together with a fragment of a greater omentum and sent for histopathological examination (Fig. 2). The microscopic image of all the collected lesions corresponded to the normal spleen tissue. The patient was discharged in a good general condition.
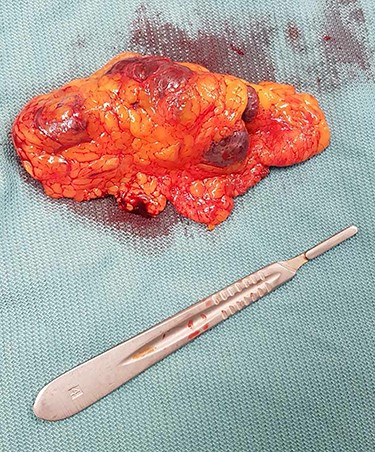
The conglomerate of tuberous lesions with a fragment of a greater omentum.
DISCUSSION
Splenosis is an autotransplantation of splenic tissue after splenectomy or traumatic rupture of the spleen. Implants can be located throughout the body, most often in the peritoneal cavity [2]. In our case, the lesions were located mainly in the greater omentum. Less frequent locations include pleural and retroperitoneal cavity, pelvis, subcutaneous tissue, kidney, liver and even cerebrum [2–5].
The incidence of abdominal splenosis ranges from 16 to 67% [1]. Extraabdominal locations are much rarer [6, 7]. The time interval between spleen injury and diagnosis of splenosis ranges from 5 months to 32 years (average 10 years) [2, 3, 7]. Interestingly, in our case this period was longer (over 40 years).
The name ‘splenosis’ was proposed by Buchbinder and Lipkoff in 1939. However, the first description appeared much earlier. In 1883, Griffini and Tizzani noticed splenosis in dogs. The first cases in humans were recorded only in 1896 by Albrecht and in 1907 by Schilling. [8].
So far, several mechanisms explaining the pathogenesis of splenosis have been proposed. The main one is the spread of damaged splenic tissue into surrounding cavities. However, it does not explain the extraabdominal locations. Therefore, the hematogenous dissemination is considered as a second mechanism. The latest theory assumes that in response to tissue hypoxia, spleen erythrocyte progenitor cells enter the liver through the portal vein where they then grow [5, 6, 8].
Most patients with splenosis are asymptomatic. It is usually found accidentally, during physical or imaging examination, autopsy or abdominal surgery for another reason [7, 9, 10]. That was the case with our patient who had the splenosis discovered during diagnosis for nephrolithiasis. The symptoms may include nonspecific abdominal pain, palpable abdominal mass, gastrointestinal or intraabdominal hemorrhage, bowel obstruction or hydronephrosis [2, 3, 10]. Spleen implants remain functional, which can have positive and negative implications. An unfavorable consequence is the possibility of recurrence of the disease that was the cause of previous splenectomy. On the positive side, this might reduce the risk of severe infections caused by capsular bacteria, including sepsis [3, 4, 7].
The differential diagnosis is important, because splenosis may mimic serious diseases such as metastatic cancer, lymphoma, primary liver or renal cancer. Accessory spleens, endometriosis, hemangiomas, multiple adenomas, granulomatous diseases, reactive adenopathy or peritoneal mesothelioma should also be taken into account in the differentiation [3, 4, 9].
Because of the lack of symptoms, the diagnosis is often accidental. A peripheral blood smear may show absence of typical post-splenectomy hematological markers such as Howell–Jolly bodies or siderocytes, an increase in reticulocyte count, or protective pneumococcal antibody levels in an unvaccinated person [3, 4, 6, 7]. Common imaging tests, such as ultrasound or CT, have a limited diagnostic value in this disorder [4, 7]. The gold standard method is radionuclide imaging using Tc-99 m-labeled and heat-damaged erythrocytes [5, 6]. In doubtful cases, histopathological examination is recommended [3]. Despite the possibility of diagnosis using noninvasive tests, splenosis is still often diagnosed using histopathological examination. Due to the suspicion of a neoplastic process based on changes in CT and limited access to scintigraphic examinations, the same was done in our case.
After the diagnosis has been confirmed, no further treatment is required, except for symptomatic patients [7]. Surgery is indicated in all patients with symptoms or complications, in case of an uncertain diagnosis and suspected neoplastic process [4, 6].
CONCLUSION
Due to the increase in the number of road accidents and traffic injuries, splenosis is becoming an increasingly common phenomenon, which is why it seems important to disseminate knowledge about this condition. It is worth taking abdominal splenosis into consideration during the differential diagnosis of tumor-like lesions that suggests a neoplastic process, especially in patients with a history of splenic trauma or spleen removal in good general condition. Consequently, unnecessary surgery can be avoided in many cases. Furthermore, confirmed splenosis should be clearly recorded in the patient’s medical history to prevent possible diagnostic dilemmas in the future.
CONFLICTS OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- traffic accidents
- autopsy
- differential diagnosis
- laparotomy
- neoplastic processes
- rupture
- splenectomy
- splenosis
- surgical procedures, operative
- transplantation, autologous
- abdomen
- diagnostic imaging
- neoplasms
- spleen
- surgery specialty
- spleen injuries
- urinary tract computed tomography
- intraperitoneal infusion
- histopathology tests
- incidental findings
- lymphadenopathy



