-
PDF
- Split View
-
Views
-
Cite
Cite
Monica E Rebielak, Mary R Wolf, Rebecca Jordan, Jacqueline C Oxenberg, Adrenocortical carcinoma arising from an adrenal adenoma in a young adult female, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz200, https://doi.org/10.1093/jscr/rjz200
Close - Share Icon Share
Abstract
Adrenocortical carcinoma (ACC) is a rare malignancy that often carries a poor prognosis whereas adrenal incidentalomas are relatively common findings on imaging. Although most adrenal lesions are benign, 15% of patients with ACC are diagnosed based on workup for an adrenal incidentaloma. Continued surveillance or surgical resection may be recommended depending on size. The risk of a benign, non-functional adrenal lesion becoming malignant is low. Therefore, adrenal lesions typically undergo surveillance for no more than 2 years in patients with stable findings and no history of malignancy. This case describes a young adult female with a benign left adrenal adenoma who was found to have high grade ACC 7 years later. Based on interval size increase with indeterminate density, patient underwent surgical resection with adjuvant radiation and medical therapy.
INTRODUCTION
Adrenal tumors are common findings on imaging performed during the workup of an unrelated complaint. These are referred to as adrenal incidentalomas and can be found in 3–10% of the population [1]. Classification includes functional status where most lesions are clinically silent. Functioning tumors can undergo further endocrine testing to delineate underlying causes including pheochromocytoma, Cushing’s syndrome, and primary hyperaldosteronism [1]. In contrast, ACC is a rare malignancy that has a reported incidence of 0.7-1.5 per 1 million people per year [2]. The majority of patients are between the ages of 40-50 with a minor peak among children less than 5 years. ACC occurs more frequently in women than men, with a ratio of 1.5-2.5:1 [2]. Frequently patients with ACC present with advanced disease which is associated with poor outcomes and decreased survival. Since surgical resection remains the definitive treatment, early detection is a critical factor.
CASE REPORT
A 27-year-old Caucasian female with a past medical history significant for untreated hypertension, irritable bowel syndrome, hidradenitis, and ovarian cysts presented to the emergency department for evaluation of a three-day history of left flank pain. She had a prior CT scan seven years prior at which time a 2.7 × 2.1 cm left adrenal lesion, consistent with an adenoma, was found (Fig. 1). At recent presentation, non-contrast CT scan of the abdomen and pelvis was performed, demonstrating a 5.6 × 3.7 × 4.0 cm mass contiguous with the left adrenal gland and splenic artery (Fig. 2). She was ultimately discharged home with recommendation for further outpatient workup. Subsequent CT of the abdomen and pelvis with IV contrast revealed a 5.0 × 6.2 cm left adrenal mass. Portal phase density was 67 HU with washout seen at 15 minutes with HU of 42. MRI of the abdomen with adrenal protocol was then performed, depicting a 4.7 × 5.9 cm enhancing left adrenal mass with a differential diagnosis of pheochromocytoma, adrenal carcinoma, and metastatic disease. Biochemical workup was unremarkable aside from an elevated total/free testosterone of 124 ng/dl and 17.2 pg/ml. However, a diagnosis of polycystic ovarian syndrome was discussed with her in the past. The patient was then seen in the surgical oncology clinic at which time she complained of persistent left flank pain with no abnormal findings on physical examination. Surgical resection was recommended and patient underwent a robotic assisted laparoscopic left adrenalectomy. She had an uncomplicated post-operative course and was discharged home the following day. Surgical pathology revealed a high grade ACC measuring 8.4 cm in greatest dimension. There was invasion into the adrenal capsule and presence of small vessel lymphovascular invasion. Surgical margins were uninvolved with distance to closest radial margin of one mm. Immunostain showed significantly elevated Ki-67 labeling index up to 30% in focal areas of the tumor. The tumor also showed focal mitotic activity ranging from 0-4 mitoses/HPF, resulting in a diagnosis of high grade ACC. This case was discussed at a multidisciplinary meeting and adjuvant treatment was recommended. She then received external beam radiation to the left adrenal bed with a total dose of 5040 cGy at 180 cGy/F. She established care with medical oncology and was started on Mitotane with a goal dose of 6000 mg/day and goal level of 14-20 mcg/mL.
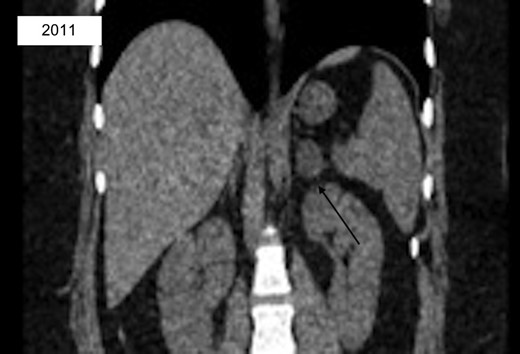
CT abd/pelvis with incidental finding of left 2.7 × 2.1 cm low-density adrenal lesion consistent with adenoma.

CT abd/pelvis revealing interval enlargement with heterogeneous density, now 5.0 × 6.2 cm with eccentric hyperdense region.
DISCUSSION
We present a rare case of ACC in a young patient with a prior nonfunctioning, benign adrenal adenoma. While a small percentage of patients with ACC are diagnosed based on workup for an incidentaloma, very few similar cases have been seen [3]. Her original imaging was suggestive of a benign adrenal adenoma but was ultimately found to have a high grade ACC without any component of adenoma 7 years later. While progression from adenoma to carcinoma can be suggested, this is likely not the case since most reported adrenal incidentalomas are benign. Additionally, only 5% of patients with ACC have a disease course > 10 years so it may not have been detected during the recommended 2 year follow-up surveillance [2].
CT characteristics can be helpful in determining the risk of malignancy, particularly if the lesion is greater than 6 cm. Management of nonfunctioning adrenal masses relies on the distinction of malignant vs. benign tumors. A traditional predictor includes size, where the risk of ACC is less than 2% in tumors under 4 cm. Once an adrenal mass reaches greater than 6 cm, the risk of malignancy rises to 25% [2]. While this patient’s lesion measured over 6 cm on preoperative imaging, ACC was not highly suspected given the patient’s age and history of ipsilateral benign adrenal adenoma. Median age at diagnosis of ACC is approximately 55, whereas our patient was only 27 years old. She was however Caucasian and female, which are common characteristics for ACC. The patient was referred for genetic evaluation and was negative for commonly associated genetic mutations, including TP53, MEN1, and Lynch Syndrome.
Even though it may be a rare event, ACC can occur in patients with prior benign, nonfunctioning adenomas well after the recommended surveillance period. Therefore, imaging should be continued as per current guidelines until more data is available to predict which patients with benign adenomas are at risk of developing ACC. Imaging characteristics can be helpful in determining the risk of malignancy, particularly if the lesion is greater than 6 cm. Ultimately, more research needs to be done to determine how long lesions should be followed before deciding that there is little to no risk of malignant potential.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest regarding the publication of this paper



