-
PDF
- Split View
-
Views
-
Cite
Cite
Rebecca M Rentea, Devin R Halleran, Hira Ahmad, Elias Maloof, Richard J Wood, Marc A Levitt, Transanal-only Swenson-like pull-through for late diagnosed Hirschsprung disease, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz341, https://doi.org/10.1093/jscr/rjz341
Close - Share Icon Share
Abstract
Hirschsprung disease (HD) is an obstructive colonic process usually diagnosed in the neonatal period. A small subset of cases are diagnosed late, present with severe constipation without enterocolitis and have low rectosigmoid disease. A transanal-only pull-through is a well-described approach but in the newborn period risks a situation whereby the transition zone is higher than the sigmoid. We present our experience with the unique patient population of older HD patients in whom the transition zone was reliably reachable via a single-stage transanal approach, performed in prone position. Patients between 2 and 6 years of age with a rectal or sigmoid transition zone and minimal proximal colonic dilation can undergo a primary transanal pull-through surgical approach.
INTRODUCTION
Hirschsprung disease (HD) is an obstructive colonic process usually diagnosed in the neonatal period. A small subset of cases are diagnosed late, present with a prolonged history of abdominal distension and constipation prior to diagnosis and have not had episodes of enterocolitis. This clinical scenario points to low (rectosigmoid) disease and is clinically a milder form of HD. A transanal-only pull-through is a well-described approach but in the typical HD patient in the newborn period risks finding a transition zone higher than the sigmoid, which is why a laparoscopic or umbilical biopsy should be the first part of the procedure. We present our experience with the unique patient population of older HD in whom the transition zone was reliably reachable via a single-stage transanal-only approach and can be performed in prone position.
CASE REPORT
A retrospective review was performed to identify all children who underwent a transanal-only pull-through following late diagnosis of Hirschsprung disease between 2014 and 2019. A late diagnosis of HD was defined in any child with HD and older than 2 years of age at the time of diagnosis. Demographics and operative details including enterocolitis episodes, fecal continence for those > 4 years of age were evaluated.
Of 54 primary cases of HD from our center, 19 (35%) were older than 2 years of age at diagnosis of HD, and we felt that 4 (7%) qualified for a transanal-only primary. Diagnoses occurred at 4.4 years of age (1.6–6.1 years). The mean symptom was constipation in all patients, and none experienced any episodes of enterocolitis (Table 1). All patients underwent a contrast enema and a full thickness rectal biopsy. The contrast enema in each patient identified a low transition zone in the distal rectosigmoid colon and no dilation of the more proximal colon (above the sigmoid). All patients were able to decompress their colon through increased use of laxatives prior to surgery.
| Characteristic measured (n = 4) | |
| Age (years, min–max) | 4.4 (1.6–6.1) |
| Gender | Male = 2, female = 2 |
| First symptom—constipation | 4 (100%) |
| Full-thickness biopsy | 4 (100%) |
| Contrast enema | 4 (100%) |
| Comorbidities | 2 (50%) |
| Operative details | |
| Age at OR (years) | 4.7 (2.0–6.4) |
| Length of case (hours) | 3 (2–4) |
| Level—rectosigmoid | 4 (100%) |
| Preoperative Length of Stay (LOS) (day) | 1 |
| Postoperative Preoperative Length of Stay (LOS) (day) | 5 (4–6) |
| Outcomes | |
| Readmissions for HAEC | 0 |
| Constipation | 2 (50%) |
| Night time fecal soiling postop | 2 (50%) |
| Laxative requirement | |
| Senna 15 mg + fiber | 3 (75%) |
| Miralax 17 g | 1 (25%) |
| Characteristic measured (n = 4) | |
| Age (years, min–max) | 4.4 (1.6–6.1) |
| Gender | Male = 2, female = 2 |
| First symptom—constipation | 4 (100%) |
| Full-thickness biopsy | 4 (100%) |
| Contrast enema | 4 (100%) |
| Comorbidities | 2 (50%) |
| Operative details | |
| Age at OR (years) | 4.7 (2.0–6.4) |
| Length of case (hours) | 3 (2–4) |
| Level—rectosigmoid | 4 (100%) |
| Preoperative Length of Stay (LOS) (day) | 1 |
| Postoperative Preoperative Length of Stay (LOS) (day) | 5 (4–6) |
| Outcomes | |
| Readmissions for HAEC | 0 |
| Constipation | 2 (50%) |
| Night time fecal soiling postop | 2 (50%) |
| Laxative requirement | |
| Senna 15 mg + fiber | 3 (75%) |
| Miralax 17 g | 1 (25%) |
| Characteristic measured (n = 4) | |
| Age (years, min–max) | 4.4 (1.6–6.1) |
| Gender | Male = 2, female = 2 |
| First symptom—constipation | 4 (100%) |
| Full-thickness biopsy | 4 (100%) |
| Contrast enema | 4 (100%) |
| Comorbidities | 2 (50%) |
| Operative details | |
| Age at OR (years) | 4.7 (2.0–6.4) |
| Length of case (hours) | 3 (2–4) |
| Level—rectosigmoid | 4 (100%) |
| Preoperative Length of Stay (LOS) (day) | 1 |
| Postoperative Preoperative Length of Stay (LOS) (day) | 5 (4–6) |
| Outcomes | |
| Readmissions for HAEC | 0 |
| Constipation | 2 (50%) |
| Night time fecal soiling postop | 2 (50%) |
| Laxative requirement | |
| Senna 15 mg + fiber | 3 (75%) |
| Miralax 17 g | 1 (25%) |
| Characteristic measured (n = 4) | |
| Age (years, min–max) | 4.4 (1.6–6.1) |
| Gender | Male = 2, female = 2 |
| First symptom—constipation | 4 (100%) |
| Full-thickness biopsy | 4 (100%) |
| Contrast enema | 4 (100%) |
| Comorbidities | 2 (50%) |
| Operative details | |
| Age at OR (years) | 4.7 (2.0–6.4) |
| Length of case (hours) | 3 (2–4) |
| Level—rectosigmoid | 4 (100%) |
| Preoperative Length of Stay (LOS) (day) | 1 |
| Postoperative Preoperative Length of Stay (LOS) (day) | 5 (4–6) |
| Outcomes | |
| Readmissions for HAEC | 0 |
| Constipation | 2 (50%) |
| Night time fecal soiling postop | 2 (50%) |
| Laxative requirement | |
| Senna 15 mg + fiber | 3 (75%) |
| Miralax 17 g | 1 (25%) |
There were 15 patients (28% of all patients and 79% over age 2 years) who did not undergo transanal-only pull-through. These patients underwent a primary pull-through using laparoscopy, and 11(58%) had a diverting colostomy/ileostomy in place at the time of pull-through. In all patients, the length of proximally dilated colon was significant and involved mobilization of the descending colon.
DISCUSSION
Late-diagnosed HD occurs in children and young adults and is defined variably as cases which are diagnosed more than 30 days after birth all the way to adulthood. Children who present with late diagnosed HD more often present with constipation as their primary symptom and almost never have enterocolitis [1]. The diagnosis is often challenging and delayed. A full-thickness rectal biopsy is diagnostic in 100% of cases, while an absent rectoanal inhibitory reflex (RAIR) was only absent on anorectal manometry (AMAN) 63.8% of the time- the rest were felt to be non-diagnostic according to the literature [2]. A meta-analysis of HD presentation after childhood demonstrated a transition zone limited to the rectum (79.6%), rectosigmoid (12.3%), descending colon (0.8%) and total colonic (0.4%) [3]. These findings imply that children diagnosed later often have a milder form and shorter segment of disease [1] as they usually do not present with enterocolitis but rather constipation [3]. The technical implications of this for the surgeon are a better prediction of the transition zone and the need to manage colonic dilatation.
Multiple operative approaches have been performed including a Soave, Swenson, Duhamel, myectomy and low anterior resection with myectomy or colectomy [4]. These surgeries include adjuncts of laparoscopy, laparotomy and transanal variations of these approaches. Diversion with colostomy (end, loop or blowhole) as well as a ileostomy have also been described as temporizing measures to help a proximally dilated colon decompress [5, 6]. Some of the greatest challenges a surgeon faces include the approach to diversion in the patient population as stomas are prone to prolapse, contain large thick bowel to decompress and mature and bleeding of the ostomy [5, 6].
There is a subset of patients in whom primary transanal pull-through in those >2 years of age at the time of surgery is possible. While a previous case series reported that 18.8% of their late-diagnosed HD patients underwent transanal primary pull-through, these authors did not describe outcomes or reasons for choosing the operative approach [7]. In case series, the characteristics of patients who were able to undergo primary transanal-only pull-through include overall earlier age (2–6 years) vs. those diagnosed later. On contrast enema, they exhibited a limited degree of megacolon (Figs 1 and 2). Proximal colonic dilation was absent in all four patients that we felt were good candidates for a transanal-only approach. However, proximal colonic dilation (proximal of the sigmoid) was visualized in 15 patients, and therefore, a transanal-only approach was not offered. The ability to identify a clear transition zone low in the rectosigmoid was also observed in each patient. Finally, the ability to empty the colon preoperatively whether through laxatives or rectal irrigations was also present.
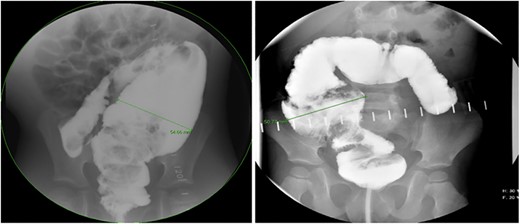
Representative contrast enema study. Note the lack of dilated proximal colon and defined transition zone in the low rectosigmoid colon. (Candidate for transanal only).
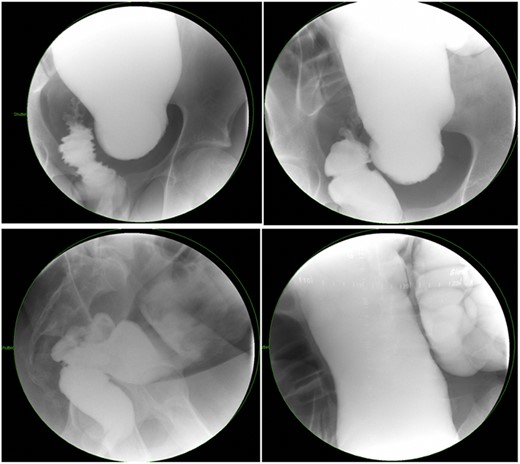
Representative contrast enema study of an older child with a large amount of proximal colonic dilation of the sigmoid and descending colon, seen here across multiple views during contrast enema (Not a candidate for transanal only).
Prior to beginning the pull-through, the colon should be irrigated to make sure that any retained fecal matter has been cleared. Careful assessment of the transition zone and confirmation of minimal proximal colonic dilatation allows for prone-only positioning and a transanal-only approach (Fig. 1). The Lone Star retractor and full-thickness dissection begin 1.0 cm proximal to the dentate line in the Swenson plane. Biopsies should be taken in a single line so as not to lose orientation [8] and 10–15 cm past the positive biopsy for ganglion cells to assure that normal caliber colon is reached before performing the anastomosis. Challenges with the transanal-only approach occur when there is a large amount of proximal colonic dilation, and therefore, in this instance, we recommend a laparoscopic approach for intraoperative mobilization of the descending and proximal colonic mobilization off the left retroperitoneum [9]. If at the time of anastomosis of the dilated ganglionated bowel, anal caliber size discrepancy is encountered a trick can be employed by placing four quadrant sutures and then bisecting each quadrant again and again with interrupted sutures [10].
Single-stage transanal-only pull-through performed in the prone position is a safe and effective option in a very small group of children diagnosed with late-diagnosed HD with transition zone in the rectum or mid sigmoid with minimal proximal colonic dilation. The advantages include single stage, ability to stay out of the abdomen and surgeon visibility.
Conflict of interest statement
All authors have no disclosures or conflicts of interest.



