-
PDF
- Split View
-
Views
-
Cite
Cite
Abdullah A Alturki, Nayf A Alshammari, Firas M Alsebayel, Ali A Alhandi, Cementless bipolar hemiarthroplasty in a patient with PMF: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz274, https://doi.org/10.1093/jscr/rjz274
Close - Share Icon Share
Abstract
Myelofibrosis is a myeloproliferative disease that falls under a group of bone marrow malignancies known as myeloproliferative neoplasms. It manifests with splenomegaly, anemia, leukocytosis and, less commonly, bone pain. Ruxolitinib, Janus kinase inhibitor, has been shown to increase survival, to improve symptoms and has the potential to decrease osteosclerotic changes. Herein, we present a case of primary myelofibrosis (PMF) in a 60-year-old female who presented with 8-month history of progressive left hip pain and later was diagnosed with pathological neck of femur fracture that was treated with cementless hemiarthroplasty. In conclusion, the use of cementless implants in hip arthroplasty in the presence of PMF has shown to be an effective and safe choice.
Introduction
Primary myelofibrosis (PMF) is a myeloproliferative disease that falls under a group of bone marrow malignancies known as myeloproliferative neoplasms. They’re collectively characterized by uncontrolled clonal proliferation of myeloid cells, which leads to progressive bone marrow scaring, extramedullary hematopoiesis and ineffective erythropoiesis [1]. The exact etiology of myelofibrosis is unknown. However, it has been proposed that myelofibrosis arises from a somatic mutation of pluripotent hematopoietic cells, which leads to chronic myeloproliferation and megakaryocyte hyperplasia [2]. Clinical picture of PMF can be varied, commonly it manifests with splenomegaly, anemia, leukocytosis and thrombocytosis [3]. Moreover, bone involvement is also seen in patients with myelofibrosis, characterized by deposition of reticulin and collagen fibers forming ostoesclerotic appearance in the bone tissue [4]. A series of case reports and literature review report that patients with myelofibrosis demonstrate an increased dual-energy x-ray absorptiometry (DXA) scan results with a mean z score of +3.8 [5]. Another study reports no significant differences between PMF patients and matched healthy adults [6].
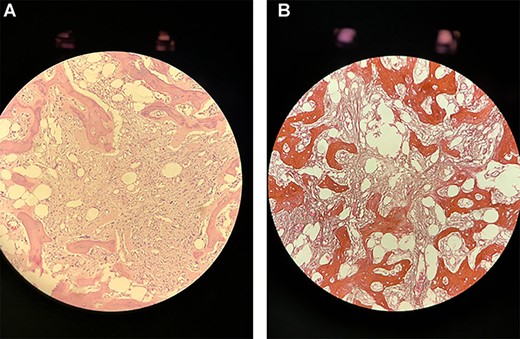
(A) A single core biopsy of bone morrow showing hypocellular morrow with extensive fibrosis and almost devoid of hemopoietic cells (B) a single core biopsy of bone morrow after the addition of Reticulin stain.
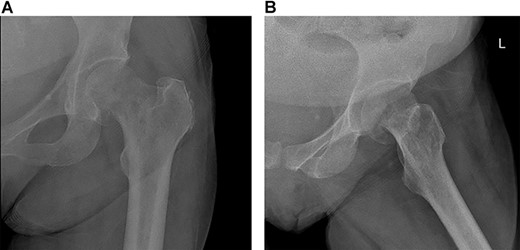
Mildly displaced fracture involving head/neck junction of the left proximal femur with suspected underlying lucency.
Brodt et al reported a case of myelofibrosis that underwent a cementless total hip arthroplasty [7], and it showed excellent outcome. Herein, we present a case of a 60-year-old female, who is a known case of PMF with a left neck of femur fracture that was treated with cementless hemiarthroplasty.

MRI showing displaced fracture noted at the left femoral neck and subcapital right femoral neck fracture with minimal reactive changes.
Case Report
A 60-year-old lady, community walker with no assistance of a cane or walker, known to have PMF on ruxolitinib. She was diagnosed with PMF in a different hospital 4 months prior to presentation (Fig. 1). She presented to our clinic with 8-month history of progressive left hip pain and was not able to bear weight since the initial episode of pain without the use of analgesia. The pain was relieved with analgesics and intra-articular injections previously, which stopped showing benefits prior to presenting to our clinic. The patient did not report any history of trauma or falling down, no fever or loss of appetite. Range of motion of the hip was severely restricted due to pain. Greater trochanter tenderness was noted on examination. Initial x-rays were ordered (Fig. 2) and revealed a possible left neck of femur fracture, which prompted us to order an MRI that showed a displaced neck of femur fracture in the left hip and a non-displaced neck of femur fracture of the right hip (Fig. 3). Surgical intervention for the left neck of femur fracture was offered to the patient, while the right neck of femur fracture was asymptomatic and conservative treatment was preferred. The patient favored surgery and requested to be done as soon as possible. She was admitted from the clinic to the ward for preoperative clearance and planning.
Initial labs were ordered for the patient. Hematology was consulted and advised to continue on the same dose of ruxolitinib. Following the clearance for surgery by hematology, the patient was taken to the operating room 6 days later.
Procedure
Under general anesthesia, a direct lateral approach (Hardinge’s approach) was used.
The fracture was immediately noted to be displaced. Femoral neck osteotomy was done with no difficulty, and the femoral head was removed. Femoral head size was noted to be 40 mm. We noted the bone quality to be excellent, similar to Brodt et al paper, which affirmed our decision to continue with the cementless system (ACCOLADE II, Stryker Inc, Mahwah, NJ, USA). However, the proximal femoral canal was completely blocked, and reaming was not possible. Multiple drilling was done gradually, and then a guidewire was inserted in the femoral canal, which opened it and allowed for the flexible reamer to be used. Biopsies were sent to pathology from the reamer and femoral head. Size 0 Accolade II stem was used with a size 22/0 mm head, and 40 mm bipolar cup to achieve excellent fixation and stable reduction.
Recovery
Postoperatively, the patient was started on a physiotherapy course consisting of non-weight bearing on the left lower limb with bed to chair mobilization. The patient achieved all her inpatient physiotherapy goals within 3 days and was discharged with her home medication and anticoagulation. During her first follow-up 3 weeks out, the surgical wound was clean, and her clips were removed.
The patient was then referred to an outpatient physical therapy center to resume her physiotherapy. The patient achieved full weight bearing and excellent range of motion within 2 months postoperatively. Implants remained in good position showing no signs of loosening on x-rays (Fig. 4) on the ninth month visit, and she denied any pain with walking and had excellent range of motion at the time.
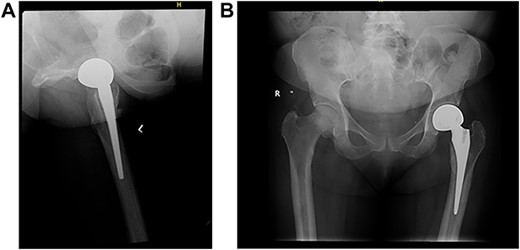
(A) Left (L) view of the implant in position; (B) Pelvic X-ray showing the implant in position.
Discussion
There are few published data about the bone morbidity of PMF. It is well-established that bone pain is a symptom of PMF. However, to our knowledge, this is the first reported case of pathological hip fracture to a myelofibrotic patient. There has been a report of postmortem findings of microfractures in a patient with PMF; however, during his lifetime, there was no radiological evidence of fractures [8].
The choice of surgical intervention between bipolar hemiarthroplasty and total hip replacement was decided based on the absence of osteoarthritic changes to the left hip, adding to that the patient’s activity level prior to her symptoms was low to begin with. The main challenge in dealing with the case was to decide whether to use a cemented versus a cementless system. There is no clear consensus on the matter due to the rarity of the disease presentation in the arthroplasty clinic [9]. However, a cementless approach was decided based on the surgeon’s preference. Additionally, we wanted to avoid unwanted side effects of femoral cementing such as increased blood loss and longer operative time [10]. Furthermore, the literature supports that cementless system in PMF is associated with an excellent long-term outcome [7], which further affirmed our decision. In conclusion, the use of cementless implants in hip arthroplasty in the presence of PMF has shown to be an effective and safe choice.
Conflict of interest statement
The authors have no conflicts of interest to declare.



