-
PDF
- Split View
-
Views
-
Cite
Cite
Sentaro Nakanishi, Hayato Ise, Natsuya Ishikawa, Daisuke Takeyoshi, Daita Kobayashi, Fumiaki Kimura, Hideyuki Harada, Hiroyuki Kamiya, Total arch replacement as treatment for repeated cerebral infarctions due to unstable plaque simultaneously in the innominate artery and left subclavian artery: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy172, https://doi.org/10.1093/jscr/rjy172
Close - Share Icon Share
Abstract
We report a case of total arch replacement in a patient who suffered repeated cerebral infarctions due to unstable plaque simultaneously in the innominate and left subclavian arteries.
INTRODUCTION
Unstable plaque or thrombus formation in arch vessels can cause repeated cerebral infarctions (CIs). In such cases, surgical replacement or endovascular treatment (EVT) of arch vessels is the therapy of choice. However, the situation is difficult if the anatomical condition is unsuitable or multivessels are diseased. Here we report a case of total arch replacement (TAR) in a patient who suffered repeated CIs due to unstable plaque simultaneously in the innominate artery (IA) and left subclavian artery (LSA).
CASE REPORT
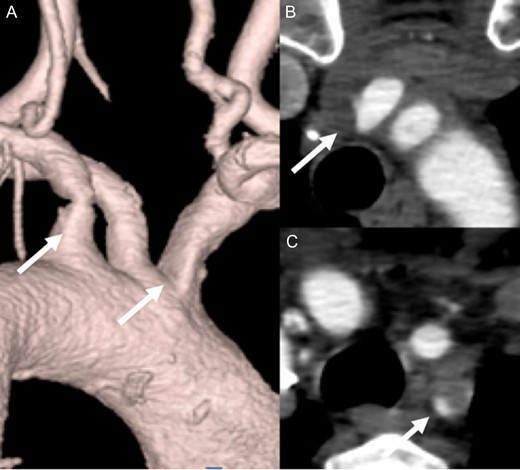
A 65-year-old woman admitted to a territorial hospital due to dizziness and listless feeling in the left arm. Magnetic resonance imaging revealed multiple CIs in the right frontal area and cerebellum on both sides (Fig. 1). Computed tomography angiography (CTA) detected stenosis in the IA and LSA (Fig. 2). No atrial fibrillation was detected despite repeated Holter-Electrocardiography. The patient was initially treated with aspirin, but thereafter experienced recurrent CIs. Clopidogrel was therefore added. Under double anti-platelet therapy, she suffered further CIs, and warfarin was added. However, CI occurred yet again. After six CIs, she was referred to our hospital.
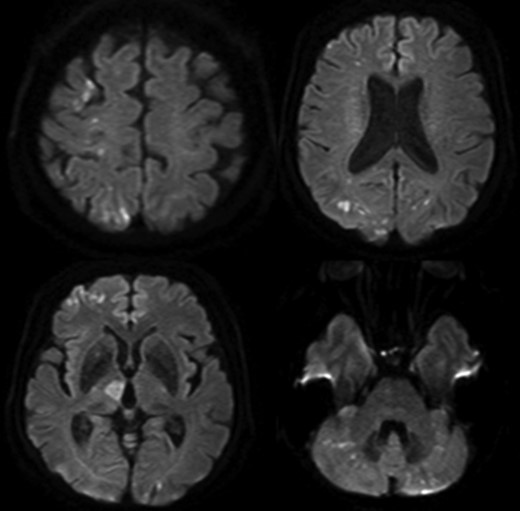
Multiple cerebral infarctions in the right frontal area and cerebellum.
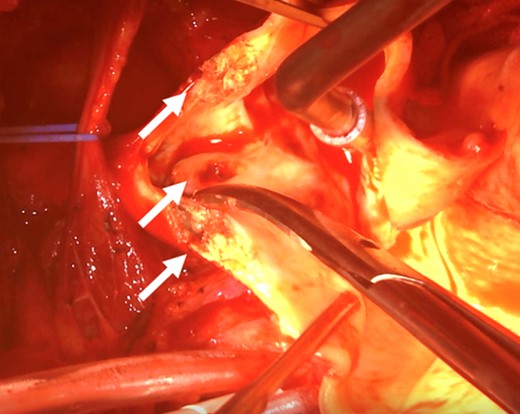
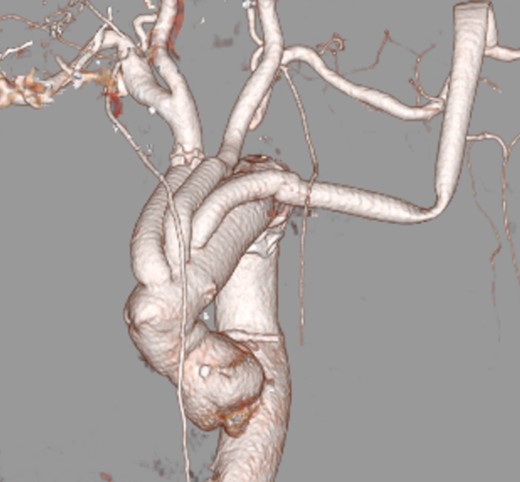
After admission, carotid ultrasonography revealed a large, soft plaque with ulceration in the IA and a very mobile soft plaque in the LSA (Fig. 3). EVT was thus considered too dangerous, and TAR using a four-branched prosthesis was planned. Intraoperatively, bilateral axillary arteries were initially exposed, and an 8-mm vessel prosthesis was anastomosed. Median sternotomy was then performed. Cardiopulmonary bypass was established with arterial perfusion via bilateral axillary arteries and bicaval venous drainage. TAR was performed under hypothermic circulatory arrest with antegrade selective cerebral perfusion, then the brachiocephalic artery and LSA were clamped and the left common carotid artery (LCA) was intubated. To avoid hoarseness due to injury of the left recurrent laryngeal nerve, a hybrid prosthesis (FROZENIX, Japan Lifeline, Tokyo, Japan) was used and a distal anastomosis was created between the LCA and LSA. The LCA was ligated and the prosthesis, which was anastomosed to the left axillary artery, was brought into the mediastinum and anastomosed with a branch of the four-branched prosthesis (Fig. 4). The postoperative course was uneventful and the patient was discharged on postoperative day 16 (Fig. 5).
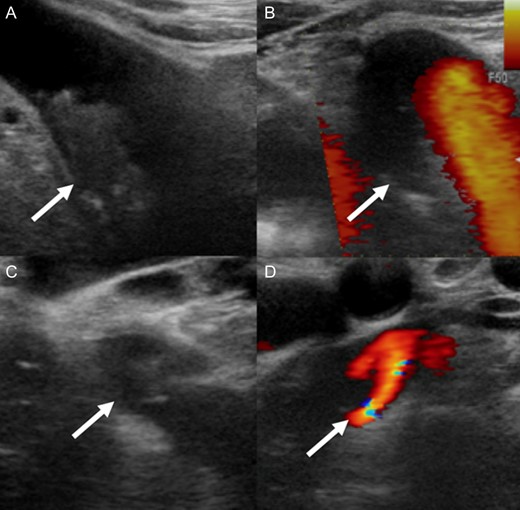
A soft plaque with ulceration in the IA (A, B) and a very mobile soft plaque in the LSA (C, D).
DISCUSSION
We reported a case of refractory CIs caused by unstable plaque in the IA and LSA. In the present case, not a less-invasive EVT, but the much more invasive TAR was chosen as the treatment with excellent outcome.
The refractory CIs in this patient was attributed to embolic events because of unstable plaque in the IA and LSA, rather than hemodynamic hypoperfusion due to stenosis. The IA had only 50% stenosis and the LSA had 75% stenosis, which may not cause such repeated CIs. Nakajima et al. [1] reported a similar case to the present patient. An 86-year-old man experienced refractory CIs and ultrasonography revealed mobile thrombus in the IA. Autopsy identified ruptured plaque in the IA that had caused thrombus formation, resulting in fatal CI. We consider that the present case developed refractory CIs through the same mechanisms.
Nowadays, EVT is the common choice for atherosclerotic occlusive disease of the supra-aortic trunks (SAT). Ben Ahmed et al. [2] performed EVT for SAT occlusive disease in 67 consecutive patients. In their report, no postoperative deaths or strokes were encountered, and they concluded EVT of proximal stenosis of SAT is a safe, reliable, and efficient technique. Similar favorable results were reported by Takach et al. and Miyakoshi et al. [3, 4] with no neurologic complications , and by Przewlocki et al. [5] with a 2.2% frequency of embolic ischemic cerebral events.
As a matter of course, however, anatomical conditions should be taken into consideration, although previous reports on EVT for SAT have been encouraging. Even Ben Ahmed et al. [2] noted that patients were indicated for conventional open surgery when complex lesions of SAT-like multilocular or highly calcified lesions were seen in their practice. Mueller et al. [6] performed a randomized controlled trial comparing carotid artery stenting (CAS) and carotid endoarterectomy (CEA) in 184 patients, with 51% of patients in the CAS group and 16% of patients in the CEA group showing new ischemic brain lesions. They concluded that complex configuration of the aortic arch and internal carotid artery tortuosity increase the risk of cerebral ischemia during CAS, but not during CEA, so vascular anatomy should be taken into account when performing EVT. The patient in the present report had unstable soft plaque in the IA and LSA. We thought that passage of a guidewire close to the plaque might represent a highly dangerous situation risking fatal CI, and therefore selected open surgery.
In the present case, TAR was performed, although several reports have described extra-anatomical bypass surgery to SAT. However, those previous studies demonstrated relatively high mortality rates of 0.5–20% and morbidity rates of 3–22% [2]. Moreover, even after extra-anatomical bypass, thrombi can grow into the aorta and cause further embolization. Considering not only the perioperative risks, but also the potential future risks of extra-anatomical bypass, we consider the risks associated with TAR as acceptable.
In conclusion, we have reported the case of a patient who underwent TAR for the uncommon situation of refractory CIs caused by unstable plaque in the IA and LSA. Our case suggests that TAR may be a suitable choice in patients having SAT disease with a very complex anatomical configuration.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
All authors declare they have no conflict of interests.
FUNDING
None of authors received any funding.



