-
PDF
- Split View
-
Views
-
Cite
Cite
Stanislav Ryndin, Andrew Delozier, Michael Stanley, After a punch: recurrence of compartment syndrome following minor trauma, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy011, https://doi.org/10.1093/jscr/rjy011
Close - Share Icon Share
Abstract
Acute compartment syndrome (ACS) is a diagnosis that requires high-clinical suspicion especially in cases when the initial causal event could be considered insignificant. We present a novel case presentation of ACS associated with minor trauma in a patient with a previous history of compartment syndrome in the same extremity from a motor vehicle accident 10 years prior to presentation. To the best of our knowledge, this is the first reported case of recurrent ACS. Due to the possibility of significant morbidity, including loss of limb, it is imperative to recognize the presentation quickly so proper surgical intervention can occur. This case shows compartment syndrome can occur after a low impact mechanism of injury and previous compartment syndrome may be a risk factor, lowering the threshold for a re-occurrence. Serial exams and compartment pressure measurements should be used to aid recognition in ambiguous clinical presentations.
INTRODUCTION
Acute compartment syndrome (ACS) is an increase in pressure of a closed fascial space that is significant enough to compromise perfusion to tissues enclosed in that space. To avoid neurovascular complications, emergent fasciotomy is imperative for relieving that pressure. Compartment syndrome is normally associated with a high energy traumatic event but multiple reports have noted cases that show a multifactorial causation. Understanding all the possible associated factors is important for maintaining high-clinical suspicion so the emergent nature of these cases can be realized. This case shows a high energy mechanism of injury is not always needed and the possibility that previous history may be associated with an increased risk of future compartment syndrome.
CASE REPORT
A previously healthy male in his 30s presented to the emergency department with a 2-day history of pain and swelling in his right upper extremity after striking a heavy bag with an uppercut punch. At the time of event, the patient felt a sudden sharp pain radiating from the wrist to the elbow, which eventually localized to the elbow. Over the next 2 days, the patient gradually developed swelling and diffuse erythema from the proximal aspect of the right arm to the wrist, tension, and decreased elbow, wrist and finger mobility. He reported a history of compartment syndrome requiring fasciotomy in his right distal arm and proximal forearm due to an automobile accident-induced crush injury 10 years prior. On exam, he was tender to palpation, weak to grip, but had intact sensation and vasculature. Initially, cellulitis was suspected, partly because of the appearance of his extremity and an unlikely traumatic mechanism for ACS. Radiographs were unremarkable for fractures. Magnetic resonance imaging (MRI) revealed extensive edema in the proximal brachioradialis muscle and extensor carpi radialis longus muscle, as well as increased signal in the extensor musculature at the dorsal aspect of the arm, but no fracture or tendinous, ligamentous or muscular tear (Fig. 1). Ultrasound showed a non-occlusive thrombus in the right axillary and brachial veins, for which the patient was eventually started on anticoagulation. All initial labs were unremarkable except the CPK of 973 and the patient was subsequently admitted.
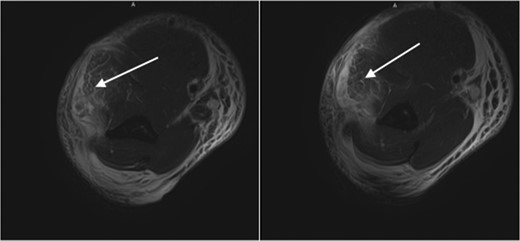
White arrows: high-grade muscle strain of the muscles the dorsal compartment with extensive soft tissue edema throughout the arm.
On hospital Day 4, due to lack of improvement on antibiotics, worsening of pain and growing suspicion for ACS, the patient was taken to the operating room (OR). After dissection of the fascia, it was found that the muscles of the mobile wad had a dark and dusky appearance along with an associated hematoma, consistent with the diagnosis of ACS. The hematoma was evacuated and vacuum assisted closure of the wound was performed (wound VAC). Four days later, the wound was re-examined in the OR, and the muscles looked pink without signs of necrosis. The wound VAC was removed and the incision was primarily closed. During his stay, the patient developed acute renal failure presumed to be due to rhabdomyolysis-induced myoglobinuria. The renal failure subsequently resolved and the patient was discharged home with no residual symptoms.
DISCUSSION
ACS is a rare condition with a disproportionately higher annual incidence in males than in females [1]. Fracture is the most common inciting event, with about 83% of ACS cases in adults preceded by fractures, most commonly tibial [2]. Other factors associated with the development of ACS include crush injuries, bleeding disorders, anticoagulation, septicemia, animal bites, arterial damage and venous cannulation [1, 3]. The potential for significant morbidity makes it necessary for constant consideration and constitutes an orthopedic emergency. ACS can lead to complications including muscle necrosis, contractures, neurological deficits, infections, rhabdomyolysis, hyperkalemia, myoglobinuria, chronic pain and even amputation [1, 4, 5]. As the time to fasciotomy increases, the likelihood of developing these complications increases, and monitoring compartment pressures has been shown to reduce time to surgery [5, 6]. However, compartment pressures are not always monitored prior to fasciotomy, and in the cases of forearm ACS, it is monitored in only 50% of patients [5]. The other half of patients proceed to the OR based on the high index of suspicion due to clinical findings such as edema, tension to extremity palpation, and the classic six Ps of compartment syndrome—pain, paresthesia, paresis, pallor, poikilothermic and pulselessness. Edema is the only sensitive clinical finding, present in 100% of cases, while others like the six Ps have poor sensitivity [5]. Our patient presented with edema, pain out of proportion to injury, weakness and questionable tense compartment.
ACS in the forearm is most commonly caused by fractures at the distal radius (34%) or diaphysis of both radius and ulna (30%), with a third of cases not associated with a fracture [5]. A study by Hope et al. [7] found that ACS without a preceding fracture has been associated with longer times to diagnosis and operative intervention, which was the case with our patient. Given the initial impression of cellulitis, an unusual mechanism of trauma, lack of fractures and soft tissue tears and non-specific findings on exam, the diagnosis of ACS was not considered until later, as the patient was clinically worsening. Fortunately, despite a 6-day delay from the onset of symptoms to fasciotomy, the vascular compromise was not severe enough to cause tissue anoxia, as there was no gross myonecrosis on intra-op exam and no neurological sequelae. This is unusual, as a delay in over 12 h almost invariably causes long-term sequelae [8]. We suspect that this might have been due to the fact that the compartment was at least partially released with prior fasciotomy, allowing pressures to build up more gradually and hence have a less traumatic effect on enclosed muscular and neural tissue. This case shows previous history of compartment syndrome may increase the risk of recurrent episodes. It also helps to highlight the multifactorial nature of compartment syndrome and closer and/or longer observation may be needed due to the possible delay in presentation. Maintaining a high clinical suspicion along with serial exams and measuring compartment pressures in all suspected cases are important factors in preventing morbidity in these cases.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest to declare.
FUNDING
There is no financial or non-financial support to declare.
AUTHORS’ CONTRIBUTIONS
Stanislav Ryndin, D.O., primary author, literature reviewer and case organization. Andrew Delozier, M.D., co-author, literature reviewer and case organization. Michael Stanley, D.O., co-author and advisor.
DISCLOSURES
None.
CONSENT
No. All patient identifying information is removed.
DECLARATIONS
This is an original article and has not been published or submitted elsewhere.



