-
PDF
- Split View
-
Views
-
Cite
Cite
Jaideep Das Gupta, Ramses Saavedra, Sundeep Guliani, John Marinaro, Muhammad Ali Rana, Decompressive laparotomy for a patient on VA-ECMO for massive pulmonary embolism that suffered traumatic liver laceration after mechanical CPR, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy292, https://doi.org/10.1093/jscr/rjy292
Close - Share Icon Share
Abstract
Massive pulmonary embolism (PE) is an embolus sufficiently obstructing pulmonary blood flow to cause right ventricular (RV) failure and hemodynamic instability. We have utilized veno-arterial extracorporeal membrane oxygenation (VA-ECMO) for early and aggressive intervention for massive PE patients. We present a case of a 61-year-old female placed on VA-ECMO for a massive PE while presenting in cardiac arrest and receiving mechanical cardiopulmonary resuscitation (CPR) via the LUCAS 2.0 device (Physio-Control Inc., Lund, Sweden). The patient suffered a severe liver laceration secondary to mechanical CPR and required a decompressive laparotomy. This case highlights that mechanical CPR during other interventions can lead to malposition of the device and could result in solid organ injury.
INTRODUCTION
Massive pulmonary embolism (PE) is an embolus sufficiently obstructing pulmonary blood flow to cause right ventricular (RV) failure, hypoxemia and hemodynamic instability [1–4]. We have utilized veno-arterial extracorporeal membrane oxygenation (VA-ECMO) for early and aggressive intervention for massive PE at our institution [5–7]. We present a case of a patient placed on VA-ECMO for a massive PE while presenting in cardiac arrest and receiving mechanical cardiopulmonary resuscitation (CPR).
CASE DESCRIPTION
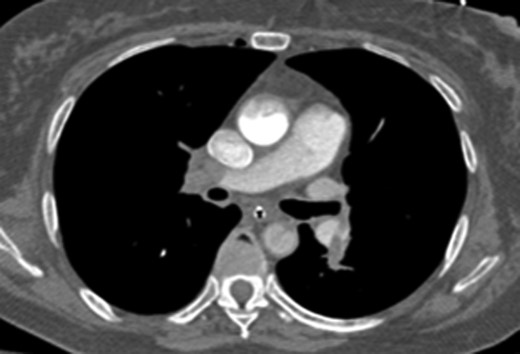
A 61-year-old female initially presented to the emergency department with shortness of breath and back pain. The patient had recently traveled to Haiti and made several trips to Denver by car. She was initially alert and oriented but sustained a cardiac arrest shortly after arrival and underwent CPR for pulseless electrical activity (PEA). Approximately 5 min into resuscitative efforts, a LUCAS 2.0 (Physio-Control Inc., Lund, Sweden) device was placed for continued chest compressions for 30 min. Bedside echocardiogram showed a dilated RV with a suspected massive PE and the ECMO team was activated. The patient was intubated and VA-ECMO access was obtained through the left femoral artery and right common femoral vein under ultrasound guidance with 17 Fr arterial and 25 Fr venous cannulas (Fig. 1). After a total of 35 min of CPR, the patient had spontaneous return of circulation.

Abdominal x-ray of VA-ECMO cannulation within the IVC and left iliac artery.
Once stable, imaging confirmed PE (Fig. 2) with a RV to left ventricle (LV) ratio of 2.1 (Fig. 3). The patient was then admitted to the ICU requiring inotropic support. Approximately 4 h later, the patient had concerning features of abdominal compartmental syndrome with increase abdominal distention and bladder pressures >25 mmHg was noted. Repeat imaging showed large volume hemoperitoneum emanating from the left hepatic lobe (Fig. 4). The patient underwent a decompressive laparotomy with a non-anatomic liver resection of segments I and II and temporary abdominal closure. Due to concerns of distal limb ischemia of the arterial cannulation site, an 8-Fr reperfusion cannula was placed in the left superficial femoral artery (SFA).
CTA chest showing significant pulmonary embolic clot burden occluding the right and left upper lung lobes.
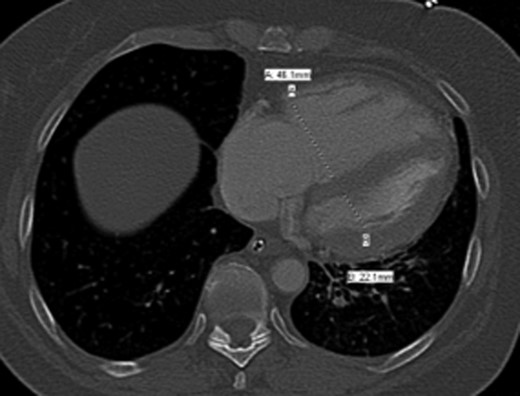
CTA chest demonstrating significant RV strain with a RV/LV ratio of 2.1.

CTA abdomen performed when the patient had abdominal compartmental syndrome requiring massive transfusion protocol. CTA showing extensive hemoperitoneum with active extravasation from the left lobe of the liver.
Post-operatively after 48 h, the patient was clinically improving with recovery of her RV function and off inotropic support. A bedside echocardiogram was performed showing an RV/LV ratio of 1.1. The patient was taken to the operating room (OR) for removal of liver packs, abdominal wall closure, decannulation of VA-ECMO, placement of IVC filter and surgical drains by the liver. The patient was hemodynamic stable post-operatively; off inotropic support and stable hematocrits. Despite physiologic improvements, she had altered mental status and left sided weakness. An MRI of the brain showed a subacute infarct of the right caudate lobe. Two days after her final operation, a repeat echocardiogram showed a normal RV functioning and RV/LV ratio of 0.7 (Fig. 5). On post-operative Day 4 the patient’s surgical drains were noted to have bloody output. Imaging showed a left hepatic artery pseudoaneurysm and underwent embolization.
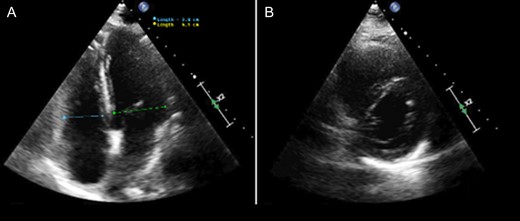
Echocardiogram performed 2 days after removal of VA-ECMO cannulation showing a normalized RV/LV ratio without evidence of RV dysfunction. (A) Four-chamber apical view. (B) Parasternal short access view.
Two weeks after the patient’s initial presentation, the patient was discharged to a skilled nursing facility and the surgical drain was removed. For outpatient follow-up, she continued to have mild left weakness and dependent on for ambulation. She was continued on Coumadin with her IVC filter remained in place after an unsuccessful removal due to thrombus burden.
DISCUSSION
Acute PE is a common event resulting in 100 000–180 000 deaths per year in the USA [8]. The majority of PE patients present minimally symptomatic and can be treated medically with solely anticoagulation with excellent short-term prognosis [2, 3]. However, there is a subset of PE (massive and submassive) that present with RV compromise [1]. Massive PE is characterized by systemic hypotension, shock and/or RV failure. The overall in-hospital mortality rates for patients with massive PE ranges from 25 to 65% despite advances in diagnosis and therapy [3, 4].
Current treatment for massive PE includes thrombolytic therapy (either systemic or catheter based), various catheter clot-retrieval techniques, surgical embolectomy and/or hemodynamic support [9]. In refractory patients, VA-ECMO has been used for salvage therapy but is associated with high morbidity and mortality. Multiple institutions have utilized an early and aggressive intervention of VA-ECMO for massive PE with encouraging results [5–7]. For our patient, we utilized early use of VA-ECMO presenting in cardiac arrest from a massive PE.
CPR-related injuries after mechanical compressions with the LUCAS device has been well-documented. Mechanical compressions are noted to have more frequent incidence of rib fractures, but no difference of sternal fractures compared to manual CPR [10]. The LUCAS device is a portable chest compression system that can provide 100 chest compression per minute with a depth of 1.5–2 inches based upon American Heart Association recommendations. However, the LUCAS system is dependent on the operator for placement of the device and therefore, malposition is a risk. For this patient, the LUCAS was positioned when VA-ECMO cannulation was performed. The LUCAS device was malpositioned with direct contact to the region of the upper abdomen during periods of CPR. Our patient suffered a grade 4 liver laceration after mechanical CPR and on anticoagulation. This case highlights that mechanical CPR during other interventions can lead to malposition of the device and could potentially result in solid organ injury.
Conflict of Interest statement
The authors report no conflicts of interest regarding the content herein.
Presentation Information
The case report has not been published or presented at any local, regional or national conference(s).



