-
PDF
- Split View
-
Views
-
Cite
Cite
Samrat Ray, Bharath Kumar Bhat, Amitabh Yadav, Samiran Nundy, Isolated dilatation of the cystic duct-Type VI choledochal cyst: a rare case presentation and review of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx067, https://doi.org/10.1093/jscr/rjx067
Close - Share Icon Share
Abstract
An isolated cystic dilatation of the cystic duct is extremely rare and very few cases have been reported in the world literature. The existing Todani's classification does not include this as a separate entity and thereby, it has been vaguely termed as a Type VI choledochal cyst by some authors in the past. We describe a case of a young male with a Type VI choledochal cyst suspected preoperatively on imaging studies and confirmed intraoperatively by laparoscopy. The cyst was localized to the cystic duct with no involvement of the common bile duct. It was excised en masse with the gall bladder by laparoscopic cholecystectomy. Considering the rarity of these lesions, an insight into the cases reported in the world is required and knowledge about the approach to managing such cases is important in surgical practice.
INTRODUCTION
Choledochal cysts are usually defined as congenital cystic dilatations of any portion of the biliary tract. They have been reported to have an incidence of 1:100 000 to 1:150 000 live births [1]. Based on their morphology and location, choledochal cysts have been classified into five major types according to Todani's classification [2]. Isolated cystic dilatations of the cystic duct are extremely rare with as few as only 20 cases reported in the world literature. The earliest description of this entity dates to 1991, with Serena Serradel et al. describing the first-ever reported case of isolated cystic duct dilatation (Type VI choledochal cyst) [3]. Here, we describe an isolated cystic duct dilatation in a young male diagnosed preoperatively and the approach to manage this rare clinical entity.
CASE REPORT
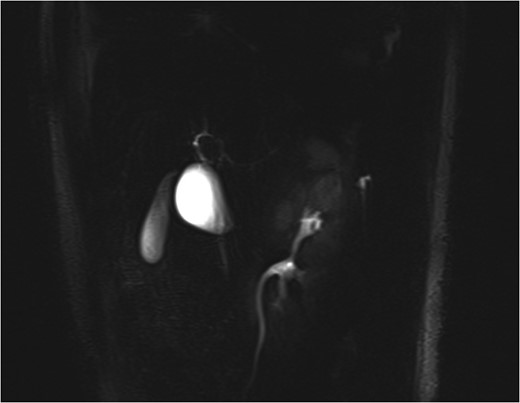
MRCP showing the cystic dilatation along the lateral wall of the bile duct mimicking a Type II choledochal cyst with GB seen separately.
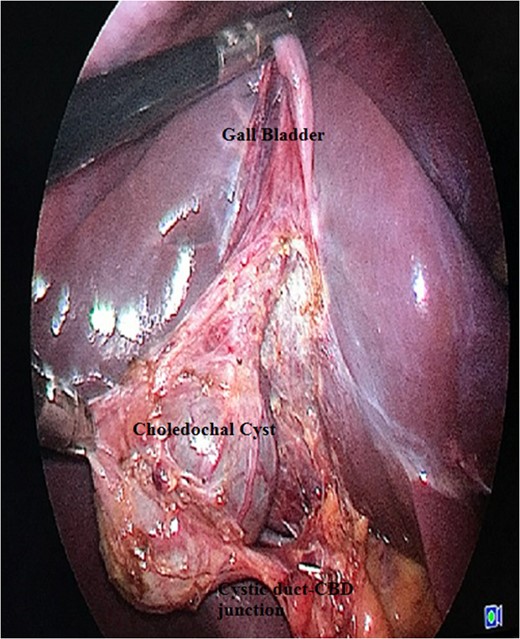
Laparoscopic view showing Calot's triangle dissected with choledochal cyst seen separately from the rest of the GB.
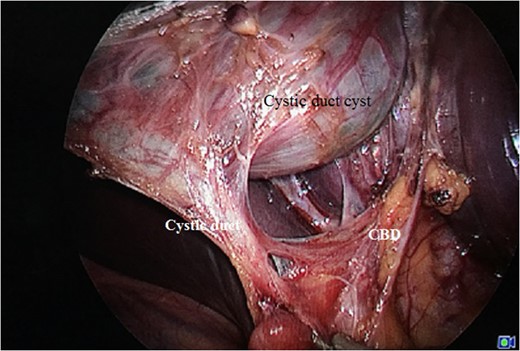
Cyst seen along with the cystic duct stalk and the arterial twig supplying the cystic duct.

Gross specimen showing the GB along with the cyst arising from the cystic duct (specimen filled with saline showing communication between the cyst and GB).
DISCUSSION
Isolated cystic duct dilatation without involving the rest of the biliary tree was not described by the Todani classification. Search into the literature revealed about 20 cases being reported from the world literature so far (Table 1).
| Author . | Year . | Age . | Sex . | Morphology . | Treatment . |
|---|---|---|---|---|---|
| Bode et al. [4] | 1983 | NA | NA | Saccular dilatation, narrow-based cystic duct | Open cyst excision with cholecystectomy with choledochoduodenostomy |
| Serena Serradel et al. [3] | 1991 | NA | NA | Saccular dilatation (preop diagnosed as Type II cyst) | Open cyst excision with cholecystectomy |
| Loke et al. [5] | 1999 | 29 y | F | Cyst compressing the CBD (Mirizzi's syndrome) | Open cyst excision with cholecystectomy with Roux en Y choledochojejunostomy |
| Manickam et al.[6] | 2004 | 20 y | F | Saccular dilatation with APBDJ | Open cyst excision with cholecystectomy |
| De et al. [7] | 2011 | 18 y | F | Fusiform dilatation of the cystic duct compressing on the CBD; cyst contained calculi within | Open cyst excision with cholecystectomy with distal CBD excision with hepaticojejunostomy |
| Shah et al.[8] | 2013 | 10 y | F | Saccular cyst of the cystic duct compressing the CBD; wide cystic duct stalk | Open cyst excision with cholecystectomy with Roux en Y hepaticojejunostomy |
| Camlidag et al. [9] | 2015 | 58 y | F | Fusiform dilatation of the cystic duct with the CBD; cholangiocarcinoma in distal part of both cystic duct and CBD | Whipple's operation |
| Nambiar et al. [10] | 2016 | 27 | M | Fusiform dilatation of the cystic duct with GB with distal CBD including intrapancreatic portion | Lap converted to open cyst excision with cholecystectomy with hepaticojejunostomy |
| Author . | Year . | Age . | Sex . | Morphology . | Treatment . |
|---|---|---|---|---|---|
| Bode et al. [4] | 1983 | NA | NA | Saccular dilatation, narrow-based cystic duct | Open cyst excision with cholecystectomy with choledochoduodenostomy |
| Serena Serradel et al. [3] | 1991 | NA | NA | Saccular dilatation (preop diagnosed as Type II cyst) | Open cyst excision with cholecystectomy |
| Loke et al. [5] | 1999 | 29 y | F | Cyst compressing the CBD (Mirizzi's syndrome) | Open cyst excision with cholecystectomy with Roux en Y choledochojejunostomy |
| Manickam et al.[6] | 2004 | 20 y | F | Saccular dilatation with APBDJ | Open cyst excision with cholecystectomy |
| De et al. [7] | 2011 | 18 y | F | Fusiform dilatation of the cystic duct compressing on the CBD; cyst contained calculi within | Open cyst excision with cholecystectomy with distal CBD excision with hepaticojejunostomy |
| Shah et al.[8] | 2013 | 10 y | F | Saccular cyst of the cystic duct compressing the CBD; wide cystic duct stalk | Open cyst excision with cholecystectomy with Roux en Y hepaticojejunostomy |
| Camlidag et al. [9] | 2015 | 58 y | F | Fusiform dilatation of the cystic duct with the CBD; cholangiocarcinoma in distal part of both cystic duct and CBD | Whipple's operation |
| Nambiar et al. [10] | 2016 | 27 | M | Fusiform dilatation of the cystic duct with GB with distal CBD including intrapancreatic portion | Lap converted to open cyst excision with cholecystectomy with hepaticojejunostomy |
| Author . | Year . | Age . | Sex . | Morphology . | Treatment . |
|---|---|---|---|---|---|
| Bode et al. [4] | 1983 | NA | NA | Saccular dilatation, narrow-based cystic duct | Open cyst excision with cholecystectomy with choledochoduodenostomy |
| Serena Serradel et al. [3] | 1991 | NA | NA | Saccular dilatation (preop diagnosed as Type II cyst) | Open cyst excision with cholecystectomy |
| Loke et al. [5] | 1999 | 29 y | F | Cyst compressing the CBD (Mirizzi's syndrome) | Open cyst excision with cholecystectomy with Roux en Y choledochojejunostomy |
| Manickam et al.[6] | 2004 | 20 y | F | Saccular dilatation with APBDJ | Open cyst excision with cholecystectomy |
| De et al. [7] | 2011 | 18 y | F | Fusiform dilatation of the cystic duct compressing on the CBD; cyst contained calculi within | Open cyst excision with cholecystectomy with distal CBD excision with hepaticojejunostomy |
| Shah et al.[8] | 2013 | 10 y | F | Saccular cyst of the cystic duct compressing the CBD; wide cystic duct stalk | Open cyst excision with cholecystectomy with Roux en Y hepaticojejunostomy |
| Camlidag et al. [9] | 2015 | 58 y | F | Fusiform dilatation of the cystic duct with the CBD; cholangiocarcinoma in distal part of both cystic duct and CBD | Whipple's operation |
| Nambiar et al. [10] | 2016 | 27 | M | Fusiform dilatation of the cystic duct with GB with distal CBD including intrapancreatic portion | Lap converted to open cyst excision with cholecystectomy with hepaticojejunostomy |
| Author . | Year . | Age . | Sex . | Morphology . | Treatment . |
|---|---|---|---|---|---|
| Bode et al. [4] | 1983 | NA | NA | Saccular dilatation, narrow-based cystic duct | Open cyst excision with cholecystectomy with choledochoduodenostomy |
| Serena Serradel et al. [3] | 1991 | NA | NA | Saccular dilatation (preop diagnosed as Type II cyst) | Open cyst excision with cholecystectomy |
| Loke et al. [5] | 1999 | 29 y | F | Cyst compressing the CBD (Mirizzi's syndrome) | Open cyst excision with cholecystectomy with Roux en Y choledochojejunostomy |
| Manickam et al.[6] | 2004 | 20 y | F | Saccular dilatation with APBDJ | Open cyst excision with cholecystectomy |
| De et al. [7] | 2011 | 18 y | F | Fusiform dilatation of the cystic duct compressing on the CBD; cyst contained calculi within | Open cyst excision with cholecystectomy with distal CBD excision with hepaticojejunostomy |
| Shah et al.[8] | 2013 | 10 y | F | Saccular cyst of the cystic duct compressing the CBD; wide cystic duct stalk | Open cyst excision with cholecystectomy with Roux en Y hepaticojejunostomy |
| Camlidag et al. [9] | 2015 | 58 y | F | Fusiform dilatation of the cystic duct with the CBD; cholangiocarcinoma in distal part of both cystic duct and CBD | Whipple's operation |
| Nambiar et al. [10] | 2016 | 27 | M | Fusiform dilatation of the cystic duct with GB with distal CBD including intrapancreatic portion | Lap converted to open cyst excision with cholecystectomy with hepaticojejunostomy |
Analysis of the world literature reveals a slight female preponderance affecting 18–55 years age group [7]. In most of the reported cases of Type VI choledochal cyst, the diagnosis was made intraoperatively. The most common preoperative diagnosis made in most of the reported cases was Type II choledochal cyst [3–5]. This was owing to the diverticular appearance of the cyst in most of the cases with proximity to the CBD.
There may be different morphologies of Type VI choledochal cyst. It may be a fusiform or saccular dilatation limited to the cystic duct alone or also involving the CBD in its distal portion or at the site of insertion of the cystic duct. The most commonly accepted theory of pathogenesis is the abnormal pancreatobiliary ductal junction (APBDJ) [11]. An APBDJ is observed in up to 40% of the cases of choledochal cysts. Singham et al. proposed a mechanism of wide opening of cystic duct with an acute angled insertion into the CBD and associated APBDJ to explain the pathogenesis of Type VI choledochal cyst [1]. However, no definitive theory has been proved yet.
The clinical presentation of Type VI choledochal cysts is like the other variants of choledochal cysts. Most cases are asymptomatic or may present with non-specific upper abdominal pain and associated jaundice or vomiting [1]. Loke et al. had described a Type VI choledochal cyst attached to a wide-based cystic duct with intraluminal calculi causing CBD compression, presenting with features of cholangitis [5]. The patient in the present case had bilious vomiting, which could be explained by compression of the duodenum by the cystic mass causing features of small bowel obstruction. Development of malignancy in the cyst is a rare presentation. To our knowledge, only four cases have been reported so far describing cholangiocarcinoma arising from Type VI choledochal cyst [12]. The carcinoma may be confined to the cyst alone or may involve the GB, CBD and intrapancreatic portion of the bile duct as well. A differential diagnosis of Mirizzi's syndrome needs to be kept in such presentations.
Preoperative diagnosis of Type VI choledochal cyst is challenging. Ultrasound abdomen is a good screening investigation in these patients. The cyst appears hypoechoic and well demarcated. MRCP or multi-detector computed tomography can also suggest the diagnosis preoperatively. The most common diagnostic confusion on preoperative MRCP is with a Type II choledochal cyst due to its similar morphology. The definitive anatomy may be delineated by ERCP. This is seldom performed due to its invasive nature. However, in patients presenting with jaundice and features of biliary obstruction or suspicious malignancy, ERCP is a definitive investigation to aid in diagnosis. Tc99m HIDA scan can be helpful in defining the biliary origin of the cyst. In cysts with wide-based stalk and proximity to the CBD, intraoperative cholangiogram is a useful adjunct on table to define the biliary anatomy [8–10].
The management of Type VI choledochal cyst is guided by its morphology [1–7]. The surgery recommended for Type VI choledochal cyst with a narrow-based cystic duct stalk is simple cholecystectomy with cyst excision. Wide-based cystic duct with proximity to the CBD warrants a CBD excision along with the above procedure and bilio-enteric reconstruction. Most of the authors reported in the literature have described the surgery by open or laparoscopic converted to open route. We did a complete laparoscopic mobilisation and cyst excision with cholecystectomy in the present case. Detailed assessment of the histology is important to detect any neoplastic changes. In patients undergoing CBD excision as a part of the procedure, evaluation of the margins for neoplasia is important. Proved malignancy of the cyst with CBD or GB warrants a definitive procedure in the form of Whipple's operation or radical cholecystectomy, respectively.
To summarize, choledochal cysts involving the cystic duct alone are extremely rare and knowledge of this anatomical variant is important for every hepatobiliary surgeon. Preoperative diagnosis may be challenging and requires a detailed radiological evaluation and multidisciplinary discussion between the surgeon, radiologist and the gastroenterologist. The surgical management of such cases is mostly guided by the morphology of the cyst and ranges from simple cholecystectomy to biliary resection procedures.
ACKNOWLEDGEMENTS
Department of MRI, Sir Ganga Ram Hospital, New Delhi.
Department of Histopathology, Sir Ganga Ram Hospital, New Delhi.
Funding
None.
CONFLICT OF INTEREST STATEMENT
None declared.



