-
PDF
- Split View
-
Views
-
Cite
Cite
Bapuji S. Gedam, Quraysh S. Sadriwala, Prasad Y. Bansod, Chronic pancreatitis with acute obstructive suppurative pancreatic ductitis: a rare case report, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx034, https://doi.org/10.1093/jscr/rjx034
Close - Share Icon Share
Abstract
Acute obstructive suppurative pancreatic ductitis (AOSPD) is a rare complication of chronic pancreatitis that has been described in only seven previous case reports since 1995. We report a case of a 33-year-old female a known case of chronic pancreatitis with computed tomography suggestive of dilated main pancreatic duct with multiple calcifications. On exploration, pancreatic duct aspiration revealed frank pus. Pus was drained after opening the pancreatic duct and longitudinal pancreaticojejunostomy was done. Patient was relieved of her symptoms after surgery. In conclusion, AOSPD should be considered in long standing cases of chronic pancreatitis. AOSPD appears to respond quickly after drainage procedure like longitudinal pancreaticojejunostomy and should be considered the treatment of choice.
INTRODUCTION
Acute obstructive suppurative pancreatic ductitis (AOSPD) is a rare complication of chronic pancreatitis that has been described in only seven previous case reports since 1995 [1]. AOSPD is defined as suppuration from the pancreatic duct; however, in contrast to the pancreatic infections that typically complicate chronic pancreatitis, it is not associated with pancreatic pseudocyst, abscess or necrosis [2]. We report a case of chronic pancreatitis with AOSPD and discuss its management.
CASE REPORT

Radiograph showing multiple radio-opaque shadows corresponding to the distal part of pancreas.

Intra-operative photograph showing frank pus on opening of pancreatic duct.
On August 2015, patient underwent endoscopic retrograde cholangio-pancreatography (ERCP)-guided stone removal with common bile duct (CBD) stent placement at other center. After 10 days of ERCP stenting, patient underwent Laparoscopic Cholecystectomy. ERCP-guided CBD Stent was removed after 6 weeks.
Two months later, patient came back with fever and pain in epigastric region with multiple episodes of bilious vomiting. On examination, there was tenderness all over the abdomen. Her blood reports were normal. Ultrasonography suggested chronic pancreatitis with shrunken pancreas with multiple calcifications in main pancreatic duct. Patient was taken for exploratory laparotomy.

CT scan showing multiple conglomerated calcifications at the tail of pancreas.
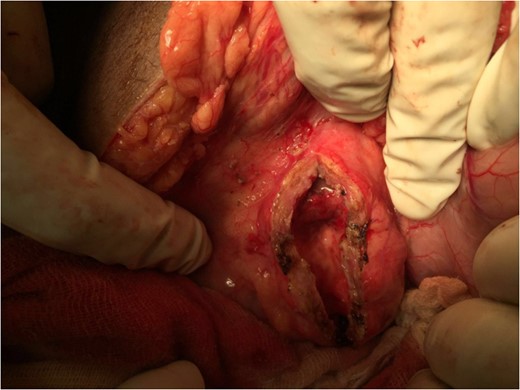
Intra-operative photograph showing main pancreatic duct after draining the pus.
Post-operatively, she had uneventful recovery. She was started on Pancreatic Lipase 25 000 IU twice daily for additional 3 months. Patient has been on 3-month follow-up since then and has been asymptomatic.
DISCUSSION
Chronic pancreatitis is an inflammatory and fibrosing disease of the exocrine pancreas characterized by irreversible morphological changes and permanent loss of function [3]. According to the Marseille–Rome classification of 1988, Chronic pancreatitis is used to refer to recurrent or persistent abdominal pain that is associated with irreversible and ongoing inflammatory destruction of exocrine parenchyma and, eventually, islets [3]. A new clinical entity termed as AOSPD was described by Weinman et al. [2], defining it as a rare complication of chronic pancreatitis with suppuration of the pancreatic duct not associated with pancreatic pseudocyst, abscess or necrosis. AOSPD has been described in only seven previous case reports since 1995 [2].
While the pathogenesis of AOSPD is not completely understood, chronic pancreatitis, prior sphincterotomy, pancreatic stasis secondary to pancreatic duct obstruction and diabetes mellitus have all been implicated as possible risk factors for its development [1].
Patients undergoing biliary sphincterotomy have a common or shared biliary and pancreatic sphincter; duodenal contents might also reflux into the pancreatic duct, in effect seeding the pancreatic duct. If pancreatic duct stones were obstructing the outflow of the duct, a ductal infection could result. This would be analogous to calculus obstruction of the biliary tree resulting in acute bacterial cholangitis. The normal pancreas is usually resistant to infection, presumably because of the presence of bacteriostatic and bacteriocidal agents elaborated in pancreatic secretions. A chronically diseased pancreas may be much more susceptible to infection because these same antibacterial agents may be significantly impaired or diminished. A pancreatic duct contaminated by duodenal reflux and obstructed by intraductal stones, in the setting of chronic pancreatitis, would seem a sufficient setting for the development of acute suppuration of the pancreatic duct [2].
Diabetes mellitus, while not present in our patient, predisposes patients to a variety of uncommon infections and may play an additive role in infection with Klebsiella. This bacterium is usually contracted by oral route and one can only speculate that during previous instrumentation of the ampulla of Vater, duodenal contents contaminated with this unusual organism may have refluxed into the pancreatic duct resulting effectively in seeding of the pancreatic juice. However, the presence of bacteria in the pancreatic duct is not by itself sufficient to cause suppuration [4].
Other causes of immune dysfunction have also been associated with AOSPD. Fujimori et al.[5] reported a case of AOSPD in the setting of peripheral blood stem cell transplantation for acute myeloid leukemia and subsequent chronic leucopoenia. Tajima et al. [6] described AOSPD in the setting of pancreatic cancer; as it can predispose to infection from biliary or pancreatic obstruction.
In all the reported cases the diagnosis of AOSPD was made on identification of pus in the pancreatic duct on ERCP. In our case, the diagnosis was made on exploring the main pancreatic duct before performing a pancreaticojejunostomy. In all previous cases, patients’ complaints resolved post-ERCP stent. Here, the definite treatment was a longitudinal pancreaticojejunostomy with Roux-en-Y jejunojejunostomy (Modified Puestow Procedure).
Surgery results in opening of the pancreatic capsule, which alleviates interstitial pressure, whereas longitudinal anastomosis ensures full drainage of the whole pancreatic duct length [7].
As AOSPD is a rare complication of chronic pancreatitis it should be kept in mind while coming across cases with dilated main pancreatic duct and chronic pancreatitis. Once diagnosed, AOSPD should be treated with prompt intravenous antibiotic treatment with pancreatic duct decompression, which can be achieved either through ERCP stenting or surgical decompression specifically longitudinal pancreaticojejunostomy with Roux-en-Y anastomosis. Surgical management should be preferred as ERCP stenting can further lead to biliary reflux into the pancreatic duct after ERCP sphincterotomy, which lead to further infection of the pancreatic duct. AOSPD seems to respond quickly to surgery as patients are relieved of their symptoms. However, as only seven cases have been reported since 1995, there appears to be some other factors contributing to its pathogenesis. Thus, further study into this rare entity shall help provide more information in the near future.
CONFLICT OF INTEREST STATEMENT
None declared.



