-
PDF
- Split View
-
Views
-
Cite
Cite
Masato Momiyama, Fumitoshi Mizutani, Tatsuyoshi Yamamoto, Yoshinori Aoyama, Hiroshi Hasegawa, Hideo Yamamoto, Treatment of a giant inguinal hernia using transabdominal pre-peritoneal repair, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw159, https://doi.org/10.1093/jscr/rjw159
Close - Share Icon Share
Abstract
We present the case of a male Japanese patient with a giant inguinal hernia that extended to his knees while standing. A transabdominal pre-peritoneal (TAPP) repair was performed under general anesthesia. Complete reduction of the contents of the hernia was achieved within 2 h 50 min. A blood loss of approximately 700 ml was noted. The patient was discharged from the hospital on post-operative Day 12, with no recurrence of the hernia 6 months post-surgery. Factors contributing to the successful outcomes included preparation of several reduction methods before surgery, use of a large size mesh and implementation of pre-operative measures to prevent abdominal compartment syndrome. Further studies are required to evaluate the feasibility of laparoscopic repair in the management of giant inguinal hernia.
Introduction
Giant inguinal–scrotal hernias are defined as hernias that extend below the midpoint of inner thigh while standing [1]. Although the prevalence of giant hernias is extremely low, patients with giant hernias have a decreased quality of life, skin problems such as ulceration and dermatitis, dysuria and sexual intercourse failure [2].
The management of giant inguinal hernias poses a special surgical challenge due to the technical difficulty of the repair and the high risk for morbidity and mortality. The aim of this report was to present the surgical management of a giant inguinal hernia extending to the knees while standing in a Japanese patient, who was treated with a transabdominal pre-peritoneal (TAPP) repair that resulted in favorable outcomes.
Case Report
A 73-year-old man was referred to our hospital by his primary care doctor because of a bulge in his right inguinal region. The patient reported this bulge had been present since his adolescence. The hernia had been reducible until age 55, and had become irreducible, thereafter. Medical history included hypertension, diabetes mellitus, asthma and cerebral infarction. He was currently taking one aspirin daily. The patient was 159 cm tall and weighed 84 kg, with a body mass index of 32.2 kg/m2. On physical examination, the bulge in his right inguinal region was roughly the size of an infant's head and the bottom of scrotum descended to his knees in the upright position (Fig. 1). Laboratory tests indicated a hemoglobin A1C (HbA1C) concentration of 7.0% and a urine glucose concentration of 4+. Lung function tests identified restrictive lung function and pre-operative cardiac ultrasound revealed no local asynergy. Abdominal computed tomography (CT) imaging identified the sigmoid colon with a large amount of feces and the great omentum as part of the contents of the hernia (Fig. 2). Although the hernia was irreducible, the patient was planned to undergo an elective surgery for hernia repair due to absence of symptoms of incarceration. Informed consent was obtained from the patient. The patient achieved a weight reduction of 3 kg within 3 months prior to surgery.

Giant inguinal hernia at admission extending below the knee while standing.
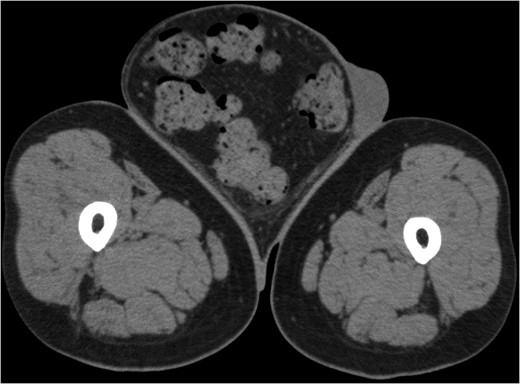
Computerized tomography image of the hernia on admission, indicating the sigmoid colon, including a large amount of feces inside the sigmoid colon, and the greater omentum as part of the contents of the hernia.
CT on the day of admission showed a hernia sac of 2263 ml, with an intra-abdominal volume of 12 021 ml. Pre-operative bowel preparation with Magcorol P reduced the volume of the hernia contents to 1604 ml, representing a 71% reduction. The intra-abdominal volume was decreased to 10 485 ml.
The TAPP procedure was performed under general anesthesia with the patient placed in a slight Trendelenburg position. In the aeroperitoneum, no adhesion between the orifice of the hernia and the abdominal content was identified. With four laparoscopic ports in place (Fig. 3), the prolapsed intestine was slowly reduced by applying external pressure to the hernia from outside of the body. Following this procedure, complete reduction of the hernia contents was achieved, with an operative time of 2 h 50 min and a blood loss of approximately 700 ml. The loss of 700 ml of blood was mainly due to the injury caused by forceps when we sought to reduce the incarcerated omentum. We did not dissect the hernia sac, leaving it with the cord distally.

Snapshot of the TAPP repair, with external compression being applied to the groin from outside of the body.
CT imaging before hernia reduction indicated the diameter of the hernia orifice to be approximately 50 mm, with the posterior wall of the hernia orifice strengthened. A mesh of sufficient area was placed to cover the orifice of the hernia, completely detaching the dorsal aspect of the hernia from the peritoneal membrane up to the dorsal ileocecal region. Given the possibility of tearing of the peritoneal membrane, a VentralightTM ST mesh (Bard Davol Inc., RI, USA), 15 cm in diameter, was used.
The patient followed a satisfactory post-operative course. The scrotum on post-operative Day 2 is shown in Fig. 4. On post-operative Day 2, the patient complained of mild abdominal fullness, which disappeared by post-operative Day 4 (Fig. 4). Ultrasonography of the lower limbs indicated absence of deep vein thrombophlebitis. The patient was discharged from the hospital on post-operative Day 12, with no recurrence of herniation, 12 months post-surgery (Fig. 5).

On post-operative Day 2, the patient complained of mild abdominal fullness with no evidence of recurrence of the hernia.

Discussion
Several options are available for the management of inguinal hernia, including watchful waiting, open repair and laparoscopic repair (TEP or TAPP) [3]. When considering surgical repair, an elective procedure is recommended, as the risk for complications associated with elective surgery are rare or minor compared to the risks associated with an emergency repair [4]. In the case of giant inguinal hernia, elective surgical repair poses a significant challenge for a surgeon due to the rarity of the condition. Although giant inguinoscrotal hernias are not a contraindication for TAPP repair, indirect reduction of the sacs can be difficult.
In our opinion, three factors contributed to the successful reduction of the contents of the hernia using a TAPP repair for our patient. First, the method of hernia reduction is an important issue to consider when performing a TAPP repair. A priori, due to the size of the hernia, we had anticipated reduction would be difficult and, therefore, had prepared several options for reducing the contents of the hernia prior to the surgery. We demonstrate that the success of combining compression from outside of the body with effective pull from inside and the additional use of ports. The second issue of importance is the selection of the mesh. We selected a large mesh, 15 cm in diameter, which would cover all areas of potential hernia defects in the groin, while still providing margins ≥3 cm from the defects. Given the possibility of tearing of the peritoneal membrane, we used a VentralightTM ST mesh for exteriorization. Third, as intra-abdominal pressure may increase suddenly after reduction of the hernia content, leading to serious complication, the risk for ACS must be considered. Symptoms of ACS include restricted lung function and deep venous thrombosis. Previous studies have shown an increased risk of ACS with a rise in intra-abdominal pressure over 25 mmHg [5]. In our procedure, we did not have the necessary equipment to monitor intra-abdominal pressure. We propose that pre-, intra- and post-operative measurements of intra-abdominal pressure are necessary to ensure safety during the reduction procedure.
Conflict of Interest Statement
Masato Momiyama, Fumitoshi Mizutani, Tatsuyoshi Yamamoto, Yoshinori Aoyama, Yoshinori Aoyama, Hiroshi Hasegawa and Hideo Yamamoto declare that they have no conflict of interest.



