-
PDF
- Split View
-
Views
-
Cite
Cite
Jessica Green, Tomoko Ikuine, Shoshana Hacker, Hernan Urrego, Karleena Tuggle, Acute small bowel obstruction due to a large intraluminal blood clot after laparoscopic Roux-en-Y gastric bypass, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw143, https://doi.org/10.1093/jscr/rjw143
Close - Share Icon Share
Abstract
Small bowel obstructions (SBOs) are a known perioperative complication of laparoscopic Roux-en-Y gastric bypass and common etiologies include internal hernia, port site hernia, jejunojejunostomy stricture, ileus and adhesions. Less commonly, SBO can be caused by superior mesenteric artery syndrome, intussusception and intraluminal blood clot. We present a case of SBO caused by intraluminal blood clot from jejunojejunostomy staple line bleeding in a patient with a normal coagulation profile. Computed tomography was used to elucidate the cause of perioperative SBO, and diagnostic laparoscopy was used to both diagnose and treat the complication. In this case, the intraluminal clot was evacuated laparoscopically by enterotomy, thrombectomy and primary closure without anastomotic revision since there was no evidence of continued bleeding. Administration of enoxaparin and Toradol post-operatively may have exacerbated mild intraluminal bleeding occurring at the stapled jejunojejunal anastomosis. Prompt recognition and treatment of perioperative SBO can prevent catastrophic consequences related to bowel perforation.
Introduction
Over 340 000 bariatric surgeries were completed worldwide in 2011, and laparoscopic Roux-en-Y gastric bypass (LRYGB) is the most common as well as technically demanding procedures performed [1, 2]. The rate of adverse intraoperative events for LRYGB has been reported at 5.5%, with a <5% risk of a major complication in the perioperative period [3–5]. Bleeding is the most common major complication requiring reoperation within 30 days (31%), followed by bowel obstruction (27%), anastomotic leak (27%) and diagnostic laparoscopy for tachycardia and abdominal pain (8%) [6]. Even more uncommon is small bowel obstruction (SBO) caused by an intraluminal clot, with a reported rate of occurrence of <0.2% in one large series [7]. We report an interesting case of SBO caused by intraluminal clot within the distal common channel.
Case Report
A 53-year-old female with a BMI of 38 kg/m2 and history of diabetes mellitus type 2, hypertension, obstructive sleep apnea and gastroesophageal reflux disease underwent an uneventful LRYGB procedure. Routine post-operative orders were placed including scheduled Toradol 30 mg intravenously every 6 hours for pain and Lovenox 40 mg subcutaneously once daily for deep venous thrombosis prophylaxis.
On post-operative day 1, she complained of nausea, vomiting and abdominal pain, though symptoms were consistent with an expected post-operative course. On post-operative day 2, however, she developed a leukocytosis of 15 600/mm3 and an intermittent tachycardia ranging from 85 to 118 bpm. An abdominal CT was obtained, which demonstrated a SBO with a transition point distal to the jejunojejunostomy anastomosis (Fig. 1). The patient was taken to the operating room for diagnostic laparoscopy. Upon initial inspection, there was no evidence of a mechanical cause for obstruction such as kinking or adhesions. However, the bowel proximal to the common channel appeared dilated and discolored (Fig. 2). Esophagogastroduodenoscopy (EGD) was performed to inspect the luminal mucosa, which was pink and well-perfused. Inspection distal to the jejunojejunostomy revealed a 50 cm section of bowel that was firm and appeared to be the point of obstruction. An enterotomy was made in the proximal common channel, which revealed a large intraluminal clot (Fig. 3). This was removed piecewise with a combination of suction and manual extraction (Fig. 4). There was no evidence of active bleeding or leakage from the jejunojejunostomy anastomosis. Due to the friability of the intestinal walls and absence of active bleeding, the anastomosis was not revised and the enterotomy was primarily closed.

Abdominal CT demonstrating SBO with a transition point distal to the jejunojejunal anastomosis.
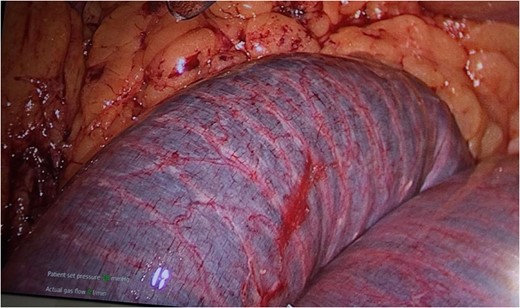
Dilated, friable small bowel of the common channel proximal to the site of obstruction with discoloration due to intraluminal clot.

Intraluminal clot within the common channel after an enterotomy was created.

Improvement in small bowel appearance after evacuation of clot with suction and manual extraction.
The remainder of the patient's hospital course was uneventful. Bowel function returned on post-operative day 4, and she was discharged home on post-operative day 5.
Discussion
While SBO due to an intraluminal blood clot has been previously reported, it is unusual [7–9]. Despite its rare occurrence, intraluminal blood clot should be considered as a cause of post-operative acute SBO. Obstructing hematomas can have severe consequences, including bowel perforation and death [10].
Most obstructions from intraluminal clot occur within 2–5 days after the bypass [8, 9]. Clot formation is commonly attributed to bleeding from anastomotic staple lines. We routinely use staples with a 1 mm staple height to create our jejunojejunal anastomosis, which is the recommended staple size for bowel anastomosis. Our patient was placed on a low enoxaparin dose post-operatively for deep venous thrombosis prophylaxis, and published reports have shown that enoxaparin at 50 mg BID does not result in increased bleeding complications after bariatric surgery [6]. Additionally, the patient received 48 hours of scheduled Toradol post-operatively, which may have contributed to staple line bleeding. However, we routinely order Toradol for post-operative pain management without ill effects. Importantly, our patient did not exhibit signs of gastrointestinal bleeding such as melena or hypotension. Mild post-operative ileus and edema at the anastomotic site may have contributed to stagnation of blood within the bowel, allowing the formation of a large intraluminal clot.
Abdominal computed tomography (CT) is an important adjunct used to diagnose SBO and can also rule out other post-operative complications such as fluid collection from anastomotic leak, abscess or extraluminal hemorrhage. While post-operative tachycardia, leukocytosis and abdominal pain are reasons for emergent diagnostic laparoscopy after bariatric procedures, in our patient CT was utilized first due to the intermittent nature of the tachycardia and the resolution of symptoms with pain medication.
Some surgeons have recommended revision of the anastomosis after the development of blood clot obstruction due to staple line hemorrhage [8]. However, we have shown that the evacuation of a blood clot by enterotomy and thrombectomy without anastomotic revision is sufficient if there is no evidence of continued bleeding. We routinely examine the gastrojejunal anastomosis with EGD while performing a leak test to ensure that there is no evidence of mucosal bleeding, but the jejunojejunostomy is beyond the reach of the EGD scope. Prior to stapling the enterotomies closed after performing the anastomosis, we examine the intraluminal surface for signs of bleeding. In this case, there were no signs of bleeding after stapling.
In conclusion, SBO from intraluminal clot formation after LRYGB is extremely rare. Administration of enoxaparin and Toradol may have exacerbated intraluminal bleeding occurring at the stapled jejunojejunal anastomosis. CT can aid in the diagnosis; however, reoperation is mandatory. Intraluminal clots can be removed laparoscopically without revising the anastomosis. Prompt recognition and treatment of perioperative SBO can prevent catastrophic consequences related to bowel perforation.
Conflict of interest statement
None declared.
References
- enoxaparin
- small bowel obstruction
- computed tomography
- hemorrhage
- surgical complications
- adhesions
- anastomosis, surgical
- blood coagulation tests
- constriction, pathologic
- hernias
- intestinal perforation
- intestine, small
- intussusception
- ketorolac
- ketorolac tromethamine
- laparoscopy
- superior mesenteric artery syndrome
- thrombectomy
- thrombus
- gastric bypass, roux-en-y, laparoscopic
- skin closures, stapled
- ileus
- symptom aggravating factors



