-
PDF
- Split View
-
Views
-
Cite
Cite
Nadja Benmohamed, Ziad Abbassi, Surennaidoo P. Naiken, Philippe Morel, Alexandra Platon, Pierre-Alexandre Poletti, Christian Toso, Management of a complex pancreaticoduodenal lesion following a suicidal attempt with a crossbow, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw212, https://doi.org/10.1093/jscr/rjw212
Close - Share Icon Share
Abstract
Traumatic pancreaticoduodenal lesions are rare, often involve a challenging management, and have high rates of morbidity and mortality. A 43-year-old male patient committed a suicidal attempt by shooting an arrow with a crossbow into his upper abdomen. He was successfully treated with cautious multidisciplinary approach. Crossbow lesions demonstrate low kinetics. Sharp tips of arrows result in localized damage, likely to involve several organs. Pancreatic lesions are of particular interest because of their difficult surgery. Surgical exploration and drainage can allow an efficient management of pancreatic penetrating lesions, even in the presence of a complete pancreatic duct disruption.
INTRODUCTION
Most abdominal traumas result from motor vehicle accident, fall, interpersonal violence and only rarely from suicidal attempt [1, 2]. The radiological assessment includes a focused assessment with sonography in trauma (FAST), and, in stable patients, an abdominal computer tomography (CT). Signs of penetrating injury, the presence of free fluid/free air, and clinical signs of guarding or shock are classical indications for a surgical exploration.
We report the case of a suicidal attempt using a crossbow directed to the epigastric area, a rare and intriguing vector of injury nowadays. It implied multidisciplinary management, especially related to the presence of a complete disruption of the pancreatic duct. Only few cases of crossbow suicidal attempts were reported throughout the world, most of which are from forensic studies, as such injuries are most often fatal [1]. Beyond the description of the case, we discuss the management of complex pancreatic lesions.
CASE PRESENTATION

Image of the patient immediately after admission, showing the entry point of the arrow in the abdomen.
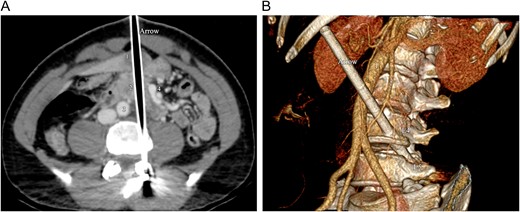
Intravenous contrast-enhanced CT of the abdomen. (A) Axial CT image shows the arrow, tracking through the liver (1), the pancreas (2) and the duodenum, between the aorta (3) and the superior mesenteric vessels (4). (B) 3D volume rendering CT reformation shows the oblique trajectory of the arrow, between the aorta (1) and the superior mesenteric artery (2). The arrow passes through the lateral aspect of the fourth vertebral lumbar body (L4) and ends into the left pedicle of the fifth lumbar vertebra (L5).
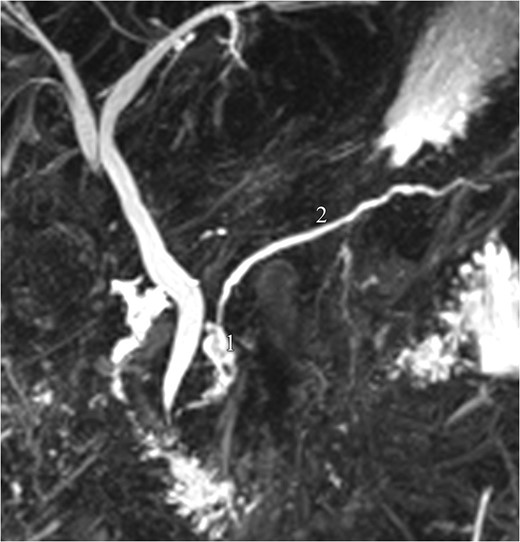
Magnetic resonance pancreatography (1 month after trauma): leak of pancreatic fluid (1), arising from the cephalic part of the main pancreatic duct (2), consistent with a ductal laceration.
DISCUSSION
Crossbows are potentially lethal weapons used for sport and hunting. In Switzerland, they can be freely purchased for private use, but are strictly prohibited in the public areas and for hunting. Crossbows have become popular and are increasingly reported in criminal acts [3, 4].
Carets and arrows usually induce very localized lesions, compared to those caused by firearms. They typically have lower kinetic energy and are fitted with a sharp end, which desiccates body tissues. On the opposite, bullets impact the body surface with a high energy, and generate tearing. Finally, the shaft of the arrow may compress surrounding wounded tissue [3].
The first step is to assess haemodynamics. The primary radiological abdominal evaluation is based on FAST echography, with or without chest and abdomen X-rays. In haemodynamically stable patients, CT has become the gold standard for early evaluation of abdominal blunt and penetrating trauma [1, 2].
Such a CT assessment is of special interest in injuries caused by arrows, such as the one of our patient. Imaging allows a precise visualization of the arrow trajectory, and enables to build detailed 3D reconstructions, which is not the case with bullet injuries.
Pancreatic trauma occurs in <5% of patients with abdominal trauma. It is complex to manage, due both to the presence of frequently associated lesions, and to its anatomical site and the nature of its parenchyma. Pancreatic trauma is associated with a high mortality and morbidity. Determining factors are the presence of associated injuries to nearby organs, vessels or bile duct, the presence of shock and time to surgery [5, 6]. Complications include fistulas, infections, pseudocysts and abscesses [7, 8]. As in the present case, combined pancreaticoduodenal injuries (PDIs) are infrequent complications, 80% of which are caused by penetrating mechanisms, and associated with high mortality rates of 18–30% [9].
Whipple's procedure has first been described in 1965 for PDI. Some advocate that it should still be performed in selected patients with trauma [9, 10]. We argue that it involves high complication rates in the emergency setting, and that therefore it should only be performed as a last resort option. Most authors nowadays support rapid, simple and damage-control surgery, showing better outcomes than complex procedures. Van der Wilden et al. showed that less invasive management was non-inferior to Whipple's procedure in a retrospective analysis of 77 patients with severe PDI [9, 10]. Our patient illustrates the management of severe PDI with simple repair and drainage.
Current recommendations for stable patients with blunt abdominal trauma are to assess injuries with a CT scan. In the case of a crossbow injury, the arrow left in the place allows precise 3D-CT reconstruction, and provides support to the medical and surgical teams. The management of multiple intra-abdominal lesions requires a multidisciplinary approach in order to elaborate the best treatment plan. Emergency Whipple's procedure remains uncommon, in favour of less invasive procedures. Simple repair, lavage and external drainage are frequently appropriate alternative options, even in the presence of a complete pancreatic duct disruption.
Conflict of interest statement
None declared.
REFERENCES
Législation suisse sur les armes, Département fédéral de justice et de police DFJP, Office féréral de la police fedpol, Confédération Suisse,



