-
PDF
- Split View
-
Views
-
Cite
Cite
Rishabh Sehgal, Cherry X. Cheung, Tristram Hills, Aqueel Waris, Donagh Healy, Tahir Khan, Perforated jejunal diverticulum: a rare case of acute abdomen, Journal of Surgical Case Reports, Volume 2016, Issue 10, October 2016, rjw169, https://doi.org/10.1093/jscr/rjw169
Close - Share Icon Share
Abstract
Jejunal pseudo-diverticulosis is a rare acquired herniation of the mucosa and submucosa through weakened areas of the muscularis mucosa of the mesenteric aspect of the bowel. They are asymptomatic in the majority of cases; however, they can present with a wide spectrum of non-specific symptoms such as chronic abdominal discomfort, postprandial flatulence, diarrhoea, malabsorption and steattorhoea. In up to 15% of cases, more serious acute complications may arise such as the development of intestinal obstruction, haemorrhage or as in our case, localized peritonitis secondary to perforation. Perforation carries an overall mortality rate of up to 40% and exploratory laparotomy followed by copious lavage with segmental resection and primary anastomosis remains the mainstay of managing such sequalae of jejunal pseudo-diverticulosis. Our case report highlights the importance of maintaining a high clinical suspicion of a perforated jejunal diverticulum in an elderly patient presenting with an acute abdomen.
Introduction
Jejunal pseudo-diverticulosis is a rare acquired fragile herniation of the mucosa and submucosa through weakened areas of the muscularis mucosa of the bowel. They are most frequently located on the mesenteric border of the jejunum and found in ~2% of small bowel contrast studies and ~5% of post-mortem studies [1, 2]. The majority of jejunal diverticulosis remain clinically silent; however, they can present with a wide spectrum of non-specific symptoms ranging from chronic abdominal discomfort, postprandial flatulence, diarrhoea, malabsorption and steattorhoea to more serious acute complications such as the development of diverticulitis, intestinal obstruction, haemorrhage or as in our case report, localized peritonitis secondary to perforation.
Case Report
An 82-year-old Caucasian male was admitted with a 2-day history of worsening lower abdominal pain associated with nausea and low grade pyrexia. His background history was significant for hypertension, benign prostatic hyperplasia, obstructive sleep apnoea, chronic obstructive pulmonary disease and dementia.
Physical examination revealed an elderly gentleman with low grade pyrexia of 37.5°C and tachycardia of 102 beats/min. On clinical examination, the abdomen was tender around the peri-umbilical and left iliac fossa region with associated guarding, but was negative for rebound tenderness and blood per-rectum. Laboratory investigations revealed a C-reactive protein of 183.4 mg/L and white cell count of 15.9 × 109/L. The remaining haematological, biochemical and coagulation profiles were all within normal limits.
An erect plain chest and abdominal radiograph was unrevealing for free air under the diaphragm and showed a non-specific bowel gas pattern, respectively. He proceeded to have computerized tomography (CT) scan of his abdomen and pelvis, which showed a hollow viscus perforation with small amount of intra-abdominal free air and intrapelvic free fluid and inflammatory change in the left paramedian mesentery (Fig. 1). The impression on CT was that this was most likely due to a diverticular perforation located within the sigmoid colon. The patient was adequately resuscitated and underwent an exploratory midline laparotomy. Intraoperative findings revealed multiple small bowel diverticulae with a large perforation of a single jejunal diverticulum without any significant gross contamination (Fig. 2). Furthermore, there was severe diverticulosis of the sigmoid and transverse colon noted. The patient underwent a small bowel resection with a primary side-to-side anastomosis and washout of the abdomen. He made an uneventful post-operative recovery and was discharged home well on Day 7.
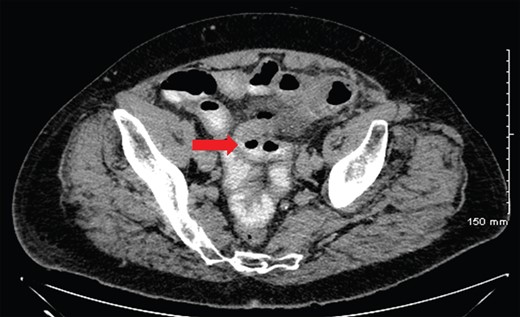
CT of abdomen with contrast revealing small pockets of intra-abdominal free air noted throughout the whole abdomen with mild fat stranding at the level of the mesenterium at the left paramedial lower abdomen and small amount of intrapelvic free fluid. A background of significant diverticular disease involving a redundant sigmoid which courses cranially to the umbilical region as well as scattered throughout the entire colon. This is suspicious for perforation within a hollow viscus (red arrow).
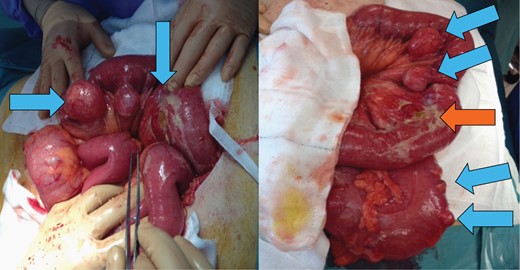
Multiple large ileo-jejunal diverticulae were found throughout the small bowel (blue arrow) and sigmoid colon. There was a perforation noted of a single large distal jejunal diverticulum (orange arrow).
Histopathological examination of the resected specimen confirmed the presence of small bowel diverticular disease. At the site of the exudates, there was prominent serosal inflammation in addition to the inflammation extending from the underlying diverticulum, with obvious intraluminal pus present. These features were in keeping with complicated diverticular disease of the small bowel with secondary perforation (Fig. 3).
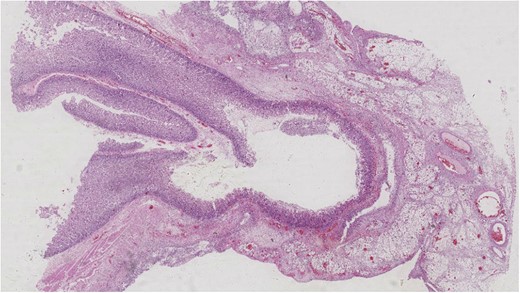
Histological examination showing H&E stained jejunal diverticulum.
Discussion
Acquired small bowel diverticulosis was first described in autopsy studies conducted by Baillie and Sommering in 1794 [3]. In 1807 Sir Astley Cooper specifically described jejunal diverticulae with 75% affecting the proximal jejunum followed by 20% and 5% in the distal jejunum and ileum, respectively [4]. These are rare entities that most commonly affect elderly males aged between 60 and 70 years. The pathophysiology of jejunal diverticulosis is largely unknown; however, it is thought to arise from motor dysfunction of the gastrointestinal smooth muscle or myenteric plexus that subsequently result in increased intraluminal pressure thereby leading to herniation of the mucosal and submucosal layers through weakened areas of the muscularis mucosa of the bowel. These false or pseudo-diverticulae are thin walled and most commonly found on the mesenteric aspect of the bowel in regions where the vasa recta penetrate the bowel wall [2]. Such small bowel diverticulae usually arise in conjunction with other coexisting diverticulae elsewhere such as the colon in up to 75% of cases which therefore may suggest a potential connective tissue link as part of the underlying aetiology. Furthermore, cocaine sniffing, use of steroids and non-steroidal anti-inflammatory drugs have also been implicated [5].
The majority of jejunal diverticulosis remain asymptomatic thereby making rates amongst populations difficult to ascertain. They are usually diagnosed incidentally on small bowel follow through studies, capsule endoscopy, CT, enteroclysis, laparoscopy or laparotomy, and autopsy. Patients usually present with a broad spectrum of non-specific symptoms including intermittent abdominal discomfort, dyspepsia, malabsorption, flatulence, diarrhoea and steattorhoea owning to bacterial overgrowth. In up to 15% of cases, patients can develop acute complications such as diverticulitis, bleeding, intestinal obstruction and like in the case of our study, perforation [6].
Small bowel perforation is associated with 40% mortality [7]. This is due to the vague clinical symptomatology and delay in making the diagnosis in a predominantly elderly demographic who often have multiple comorbidities and have a reduced ability to instigate an adequate physiological stress response that is required when undergoing surgery. Although non-operative management of a perforated jejunal diverticulum with bowel rest, antibiotics with or without CT-guided aspiration can be performed in stable patients presenting with localized abdominal symptoms and signs [8], surgical exploration, copious lavage and segmental resection with primary anastomosis remains the mainstay of management in order to avoid further contamination and sepsis. Alternative surgical modalities such as primary closure, diverticulectomy and invagination are associated with extremely poor outcome and high mortality rate and should be avoided. It is important to limit the bowel resection so as to avoid short gut syndrome and malabsorption [6, 9, 10].
In summary, jejunal pseudo-diverticulosis is a rare entity associated with a high morbidity and mortality. They are asymptomatic in the majority of cases and usually diagnosed incidentally. When symptomatic, they can present with vague non-specific symptoms or with acute complications necessitating surgical intervention. Our case report highlights the importance of maintaining a high clinical suspicion of a perforated small bowel diverticulum in an elderly patient presenting with an acute abdomen with localized signs of peritonitis. Although non-operative management has been shown to be beneficial in stable patients, surgical exploration with segmental resection and primary anastomosis remain the mainstay of management.
Conflict of interest statement
None declared.
References
- abdominal pain
- acute abdomen
- hemorrhage
- diarrhea
- flatulence
- malabsorption syndrome
- anastomosis, surgical
- diverticulum
- hernias
- intestinal obstruction
- intestines
- irrigation
- mesentery
- peritonitis
- postprandial period
- jejunum
- mortality
- mucous membrane
- diverticulosis
- older adult
- laparotomy, exploratory
- muscularis mucosa



