-
PDF
- Split View
-
Views
-
Cite
Cite
Emmanuel Katsogridakis, Hiren Patel, Ferdinand Serracino-Inglott, Nicholas Chalmers, Popliteal artery pseudoaneurysm treated with covered stent placement and thrombolysis: a case report, Journal of Surgical Case Reports, Volume 2015, Issue 9, September 2015, rjv082, https://doi.org/10.1093/jscr/rjv082
Close - Share Icon Share
Abstract
Pseudoaneurysms of the popliteal artery are a rare clinical entity, accounting for <4% of all popliteal aneurysms. Accurate diagnosis and effective intervention is required to prevent potentially limb-threatening complications. We present the case of a 37-year-old man with acute limb ischaemia due to distal calf vessel thrombosis secondary to a popliteal pseudoaneurysm that was managed with covered stent placement and thrombolysis.
INTRODUCTION
Trauma to the popliteal arteries resulting in pseudoaneurysm formation is rarely encountered outside the setting of wartime surgery [1, 2]. Its aetiology is varied and comprises blunt or penetrating trauma and iatrogenic causes.
Popliteal pseudoaneurysms (PPs) account for <4% of all popliteal artery aneurysms, and hence experience of their management in individual centres is limited [3–5]. The diagnosis of PP may also be delayed due to long-time interval between the initial trauma and symptom onset.
We present the case of a large PP causing acute limb ischaemia to a 37-year-old man.
CASE REPORT
An otherwise healthy 37-year-old man presented with acute limb ischaemia of recent onset. His past medical history was significant for smoking as well as a previous gunshot wound to the right lower limb 12 years previously that required fasciotomies.
Diagnostic work-up included an arterial Duplex scan of the right lower limb, which demonstrated a 5.5 cm × 5.2 cm aneurysm of the right popliteal artery and the lack of flow in the right anterior tibial and peroneal arteries. A CT angiogram was subsequently undertaken to establish the morphology of the aneurysm for preoperative planning, which confirmed the diagnosis but also demonstrated a large number of pellets in the soft tissues surrounding the right knee in keeping with the history of previous gunshot injury to the area. Poor opacification of the right anterior tibial and peroneal arteries was also demonstrated, suggestive of thrombosis or embolization secondary to the popliteal aneurysm.
Angiography, via an antegrade right femoral approach, showed a false aneurysm of the popliteal artery at the knee joint level. There was occlusion of the calf vessels. A 6 mm × 25 mm Viabahn (Gore) covered stent was deployed to exclude the pseudoaneurysm, and a thrombolysis catheter was left in situ in the below-knee popliteal artery (Fig. 1). Thrombolysis was started using alteplase at a rate of 1 mg/h, with a concurrent infusion of heparin 400 IU/h via the arterial sheath, as per local protocol.
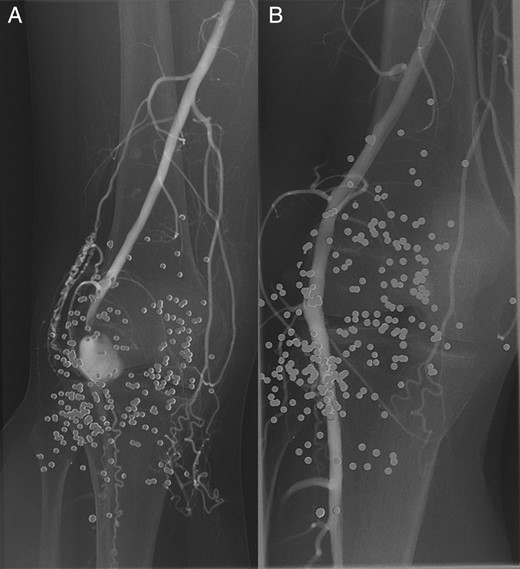
A digital subtraction angiogram of the right popliteal artery demonstrating the pseudoaneurysm, pre- (A) and post- (B) stenting. Note the numerous pellets in the soft tissues.
A repeat angiogram after 24 h of thrombolysis demonstrated improved patency while at 48 h excellent patency of the infragenicular vessels was seen (Fig. 2), and the patient was subsequently discharged on dual-antiplatelet and statin therapy. A follow-up arterial Duplex performed at 6 weeks post discharge demonstrated excellent patency of the stent graft and infragenicular arteries.
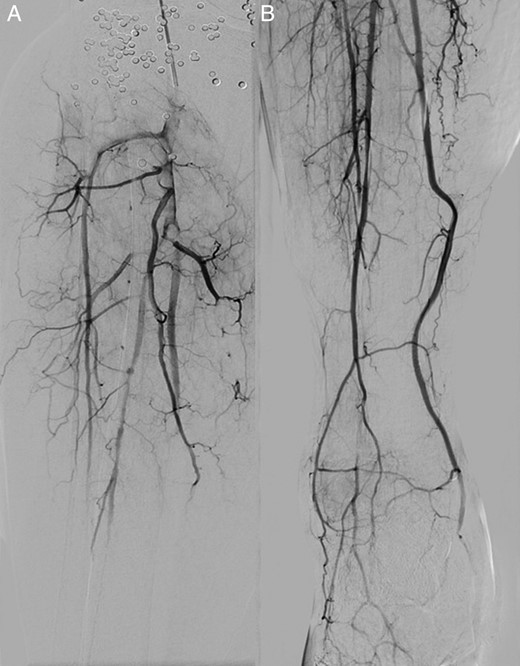
A digital subtraction angiogram at presentation (A) and after 48 h of continuous alteplase thrombolysis (B) demonstrating the improved patency of the infrapopliteal arteries.
DISCUSSION
PPs are a clinical entity that is rarely encountered in civilian medicine, and account for <4% of all aneurysms of the popliteal artery [1, 2]. Its development is considered to be secondary to the formation of a thick fibrous pseudosac following arterial wall injury and haematoma organization.
This rather slow process may explain the usual delay in diagnosis which may range from days to years, with a median delay of ∼1.5 months [6]. In our case, the delay in diagnosis was 12 years after the gunshot wound. The usual presentation is that of a painful, pulsatile mass that may have given rise to complications that may threaten limb function or viability, including thrombotic and embolic events.
A wide range of options exist for the management of PPs, including open surgical repair and endovascular treatment options. Surgical methods include the resection of the pseudoaneurysm with interposition grafting, ligation and bypass and primary arterial repair without grafting. Finally, aneurysm resection and primary end-to-end anastomosis can be considered for small aneurysms. The limiting factor, however, is the amount of perianeurysmal fibrosis and chronic inflammatory changes that are frequently encountered and hinder the safe performance of open surgical repair [1, 6].
In this case, we elected to proceed with an endovascular repair. The reasons were 2-fold: on one hand, the previous gunshot injury and the subsequent fasciotomies had led to significant deformity of the patients lower limb, while the amount of scarring would make access to the popliteal artery difficult, thus not favouring an open surgical repair. On the other hand, the distal anterior tibial and peroneal artery thrombosis would require thrombolytic therapy and thus, the endovascular approach was considered more appropriate. The false aneurysm was excluded with the covered stent prior to starting thrombolysis in order to eliminate the risk of distal embolization of thrombus from within the false aneurysm into the calf arteries during thrombolysis.
Endovascular repair has been shown to be a safe and efficient way of treating PPs associated with lower morbidity and shorter hospital stay. Careful patient selection, however, is warranted, as increased risk of early occlusion has been reported, and hence may render this approach less desirable [7, 8]. Covered stent placement was considered appropriate in this case in order to enable thrombolysis, which would not have been possible immediately after open surgical bypass.
It is unclear whether stenting in this case will be the definitive treatment, as due to the young age of the patient and the anatomical location of the stenting, stenosis or occlusion of the stent is likely in the future. To this end, the patient has been put on a surveillance programme and will be followed up closely. A short covered stent (25 mm) was used to avoid compromising future graft anastomotic sites. Thus, the endovascular treatment offered in this case was efficient in dealing with both the acute ischaemia secondary to thrombosis as well as the aneurysm itself in the short term. On the other hand, the presence of a stent does not preclude open surgery in the future, preferably in an elective setting, and this is the approach the patient selected having being informed of his options.
This case report demonstrates the efficiency of stenting in the acute management popliteal artery pseudoaneurysms with encouraging early radiological and clinical outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



