-
PDF
- Split View
-
Views
-
Cite
Cite
Kaitlin Willems, Sharon Monsivais, Hannah Vassaur, Francis P. Buckley, Single-incision laparoscopic management of a giant hepatic cyst, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv073, https://doi.org/10.1093/jscr/rjv073
Close - Share Icon Share
Abstract
Large symptomatic hepatic cysts may warrant surgical management. Traditional multiport laparoscopic technique is typically preferred over open laparotomy, but the use of the single-incision laparoscopic approach for this diagnosis is not well documented. Here, we describe the case of a 68-year-old woman who underwent complete anterior wall fenestration, excision and cauterization of a simple hepatic cyst via a single-incision laparoscopic technique through an incision at the umbilicus. The objective of this case report is to document single-incision laparoscopy as a safe, feasible and cosmetically appealing approach for the management of a large hepatic cyst.
INTRODUCTION
Hepatic cysts are not uncommon, with reported incidences ranging from 3.5 to 10% [1, 2]. Cysts are typically classified as either congenital or acquired, with simple congenital cysts presenting more commonly in women and with increased age [3]. Simple hepatic cysts are most often asymptomatic and are discovered incidentally on abdominal ultrasound or abdominal computed tomography (CT) scans [4]. When patients present with symptoms, they are usually secondary to the large size and subsequent mass effect on adjacent organs. Treatment with aspiration has fallen out of favor due to a nearly 100% recurrence rate, and more evidence is emerging that laparoscopic fenestration is a safe and effective alternative to more invasive open procedures [1, 2]. While multiple studies have shown the benefits of laparoscopic cyst management via fenestration, this procedure performed as a single-incision laparoscopic surgery (SILS) is not well described in the literature [1, 2, 4]. The goal of this case study is to demonstrate the feasibility of performing this procedure as SILS as well as its efficacy, safety and postoperative patient satisfaction.
CASE REPORT
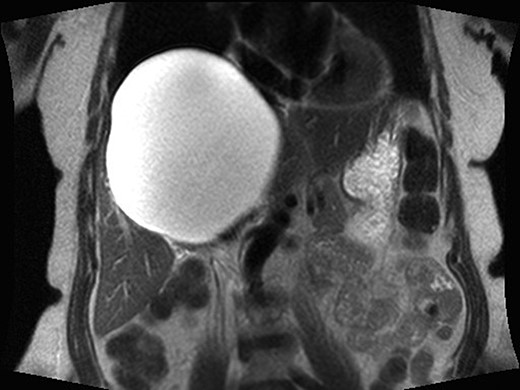
A 68-year-old female had a known hepatic cyst for about 3 years. It had been previously noted on abdominal CT but was not symptomatic at the time of discovery. Upon developing gastroesophageal reflux-type symptoms, pressure-like abdominal pain, right upper quadrant pain, fullness and nausea, she was referred for surgical evaluation. Physical exam was significant for palpable liver edge below the costal margin, but the abdomen was non-tender. This prompted further work-up, revealing elevated liver enzymes and a 16 cm × 14 cm cystic hepatic lesion on magnetic resonance imaging (MRI), consistent with a simple cyst (Fig. 1). An aspirate of the contents was obtained and sent for culture, gram stain, bilirubin, CEA levels and CA-19-9, all of which were within normal limits. Owing to the patient's discomfort, surgical fenestration and ablation of the remaining cyst wall were recommended. A single-incision laparoscopic approach was offered to the patient, and the patient consented to proceed.
The patient was taken to the operating room where a single incision through the fascia was made at the umbilicus and a SILS port placed (Fig. 2). The abdomen was insufflated and the laparoscope introduced. The liver was thoroughly inspected, and the cyst was seen in liver Segments 4, 7, 8 and superficially accessible over the caudate lobe. However, as the gallbladder was still in situ, this was not a viable location to unroof the cyst. The cyst was aspirated over Segment 8, and 1800 ml of clear aspirate was removed and sent for cytology and culture. In order to gain access to the cyst wall, a Harmonic scalpel was used; however, due to the cyst's location, this required entering between a half centimeter and a centimeter of liver parenchyma. The anterior cyst wall was excised entirely, which involved removing a 12 × 8 cm segment. An argon beam and Bovie coagulator were used to ablate the remaining cyst wall. Bleeding throughout the entire procedure was minimal. Diagnostic laparoscopy did not reveal any further areas of concern, the abdomen was irrigated and the SILS port removed. The defect was closed using a 0 Vicryl suture in a figure of eight fashion, twice. A modified wound vacuum-assisted closure dressing was placed with instructions to the patient to remove the dressing after 1 week. Total operating time was 106 min. The patient was discharged home the same day, had no postoperative pain at her 2-week follow-up visit and reported resolution of her symptoms. Furthermore, she was very satisfied with her cosmetic outcome.

Single-incision laparoscopic port inserted through the umbilicus.
DISCUSSION
The single-incision laparoscopic surgical technique has been gaining popularity in recent years. It has been stated that SILS is emerging as the latest advancement in minimally invasive surgery just as the laparoscopic technique was in 1988 [5]. Evidence is continuing to accumulate about the use of SILS in commonly performed cases such as appendectomies, colectomies and cholecystectomies [6–8]. It is proved to be safe, effective and achievable with comparable blood loss and hospital stay when compared with the traditional laparoscopic technique [9]. As SILS only requires one port insertion through the umbilicus, closure of the incision allows the potential for ‘scarless’ surgery, allowing for very cosmetically appealing results [10]. Additional studies have shown reductions in postoperative pain and reduced rates of herniation, reduced rates of wound infection and hematoma formation [10]. Continued research must be done to determine whether SILS will one day prove beneficial enough to replace traditional laparoscopic technique.
With the introduction of this new technique, surgeons must overcome a learning curve that can negatively affect operative times [7, 8, 10]. Loss of triangulation, reduced view and less space for the surgeons' hands to maneuver during operations are documented as potential difficulties with attempting the single-incision approach [10]. When laparoscopy was first introduced, significant longer operative times were the norm when compared with the traditional open approach, but this was mitigated as surgeons gained familiarity and shared standardized approaches. With increased experience with the SILS approach, standardization of technique and improved instrumentation, the challenges seen with this technique will likely be overcome as well.
This case shows that our patient was able to undergo successful cyst fenestration via SILS with a reasonable operative time and without excess difficulty or special instrumentation, thus demonstrating the flexibility of this technique. With SILS, the overall postoperative cosmetic result is superior to the traditional laparoscopic technique, as is demonstrated by postoperative patient satisfaction questionnaires [7–9]. With congenital liver cysts occurring more commonly in women, improved cosmetic outcome when addressing symptoms surgically may be an important consideration for surgeons. SILS continues to show promise and proves to be an exciting advancement in the innovative field of minimally invasive surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



